Herpes simplex virus – master of disguise and invisibility
Issue: Real superheroes
25 February 2014 article
Ask any youngster what superpowers they would like to have conferred upon them, and ‘invisibility’ would probably be high on their wish list. But some of our microbiological near-neighbours, including those living inside the majority of us right now, have already got there first.
About 80% of the population are infected, most of them unknowingly, with the herpes simplex virus (HSV), which exists in two forms: HSV-1, which traditionally causes cold sores, and HSV-2, which principally manifests ‘below the belt’; although, as my medical school textbook of pathology so memorably and eloquently put it: ‘each virus may cause disease at either site, particularly among those wont to indulge in more researche forms of sexual congress’. In testimony to this assertion, about 75% of samples collected from genital lesions that we test and diagnose in our laboratory are indeed HSV-1.
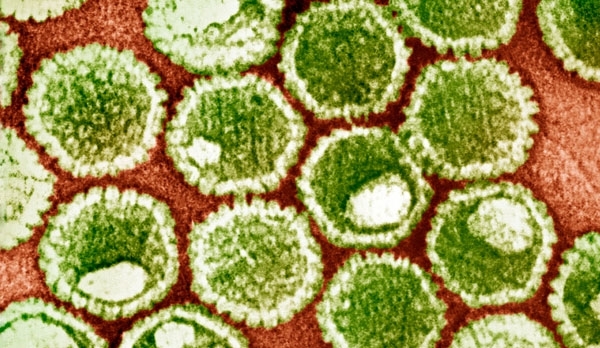
COLOURED TRANSMISSION ELECTRON MICROGRAPH (TEM) OF HSV PARTICLES
Each particle (virion) consists of a DNA core (green) surrounded by an icosahedral capsid (white), which is itself surrounded by an envelope covered in glycoprotein spikes (green outline).
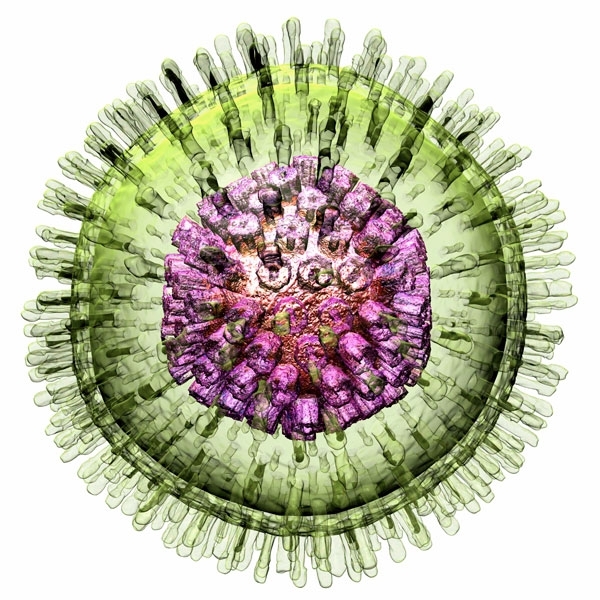
So what is this microbial invader and how does it fit the invisibility bill? HSV is a member of the herpesvirus family. Roughly spherical in shape, each viral particle measures about 1/5,000th of a millimetre across. They are surrounded by a membrane studded with proteins that work like miniature grappling hooks. These proteins enable the virus to cling to the surfaces of our cells, which are duped into drawing the attached virus inside. Once within, the genetic material of the virus is then ferried to the nucleus – the cellular headquarters – where the instructions written within the viral DNA can hijack the cell and turn it into a factory for the mass production of new herpes viruses. This is critical, because all viruses lack the machinery needed to reproduce themselves. They’re effectively infectious bags of genes that rely on breaking into cells to steal what they need.
While this might sound complex and highly evolved, from an evolutionary standpoint, herpes viruses are extremely ancient. They date from a time when host populations were comparatively small and the opportunities for infected individuals to bump into each other and swap infections were few and far between. During these times viruses such as measles, which cause severe acute infections that leave a person either dead or immune for life, couldn’t exist. They depend on a steady stream of non-immune, susceptible individuals to infect, amplify and pass on the virus. This sort of situation only arises when large, well-connected populations occur. And because, for millennia, and until only about 10,000 years ago when the concept of agriculture was invented, our ancestors lived as small, dispersed groups of hunter-gatherers, viruses like measles would have quickly burned themselves out of existence.
Instead, a clever strategy of subterfuge and stealth evolved whereby the host is turned into a healthy, lifelong viral carrier capable of transmitting the infection without even realising it. In fact, most people are surprised to learn that the majority of us pick up herpes simplex before the age of 3, usually via a kiss from a loving parent.
COMPUTER ARTWORK OF AN HSV PARTICLE
The reason we often don’t realise we’ve picked up HSV is that the first manifestation of the virus is not to cause cold sores but instead a severe sore throat, swollen lymph glands and a high temperature. When this is happening, the infecting herpes virus, which was probably shed in the saliva of a kissing contact, has invaded the epithelial cells that line the mouth and throat. Within a day or two, each infected cell has churned out thousands more virus particles, which in turn infect thousands more cells. The ensuing tissue damage and inflammation is what causes the sore throat and the high temperature, which intensifies as the immune system wades in to neutralise the invader.
But the virus doesn’t confine its activities to the lining of the mouth. This tissue is also richly supplied by sensory nerve fibres, whose job it is to detect taste, temperature and other sensations. These nerve endings are contacted and infected by virus particles budding from the overlying infected cells, providing in the process the viral equivalent of a get-away car.
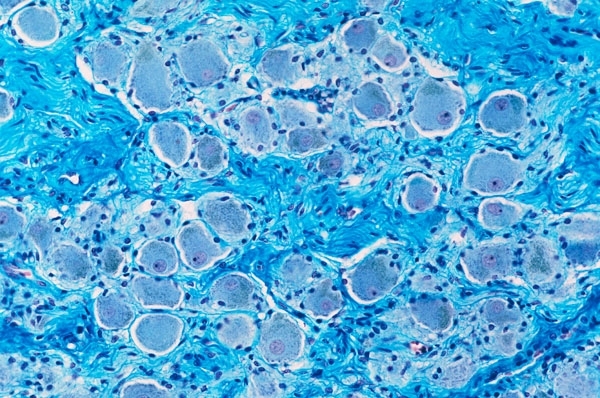
This is because nerve cells have an unusual structure. They consist of a long thin cylinder, called an axon, which measures about 1/100th of a millimetre across and can be up to many metres in length. This is connected to the ‘cell body’, which contains the cell’s DNA and, in the case of sensory nerve cells, is located alongside many other nerve cell bodies in a structure called a ganglion. The face, neck and mouth are supplied by the trigeminal nerve, and the cell bodies for these nerves sit in the trigeminal ganglion, inside the skull. Axons transmit electrical signals between the nerve endings and the cell body, which is how sensory information reaches the brain. But axons also contain a transport system, resembling a railway, which can carry cargo back and forth from the one end of the nerve to the other. Infecting HSV particles jump aboard this ‘axonal transport train’ and are carried away from the war zone in the mouth towards the distant relative calm of the cell body, in the trigeminal ganglion.
In nerve cells, HSV behaves differently. Rather than activating its replication systems to reproduce more viral particles, instead, when it reaches the cell body, the viral DNA slips quietly into the nerve cell nucleus, twists itself into a small circle of DNA and lies low. Only one or two viral genes remain active, and none of these, we don’t think, make any proteins. This state is called latency, and the virus can remain like this for the rest of an individual’s life; hidden, invisible and beyond the reach of the immune system inside the body’s own cells and with no proteins being manufactured that could give the game away.
SECTION THROUGH A NERVE GANGLION SHOWING CLUSTERS OF NERVE CELL BODIES
But lurking, concealed like this, isn’t helpful when it comes to spreading to another individual. For that to happen, the virus needs to ‘reactivate’. Virologists don’t know exactly what triggers this process, but it seems that HSV can pick up on signals inside its host nerve cell regarding what’s happening in the rest of the body. Trauma to the skin, other infections, menstruation and immune-disabling drugs and diseases (like HIV) can all provoke the virus to reactivate.
When this happens, the virus switches on its replication genes, which press-gang the host neurone to begin building a clutch of new virus particles. Once assembled, these are exported back down the axon, using the same fast axonal transport system that first brought the virus in, to the nerve ending in a patch of skin on the lips or mouth. There, the viral particles bud off, infect and replicate within the overlying skin cells, producing a cold sore blister, crammed with infectious viral particles. And because this is happening within the skin, the process can outrun the immune system, meaning that the blister can release infectious virus onto the skin surface – and then onto another susceptible individual – before any antibodies are on the scene.
But, I hear you ask, surely cold sores cannot be the only way the virus spreads, otherwise people would avoid each other whenever they saw one? You’re right, and for this reason, HSV has a further trick up its sleeve. It can also be shed asymptomatically, in body fluids like saliva. We think that perhaps a third of HSV carriers regularly ‘dispense’ infectious virus in this way. Under these circumstances it might be that the virus has produced a small sub-clinical reactivation resulting in a lesion or ulcer in the mouth. This releases viral particles that wash around in saliva and can be passed on during a kiss…
CHRIS SMITH
Consultant Virologist, Cambridge University & Addenbrooke’s Hospital, & Managing Editor, The Naked Scientists (www.thenakedscientists.com), Department of Pathology, University of Cambridge CB2 1QP, UK
[email protected]
Image: Coloured transmission electron micrograph (TEM) of HSV particles. Each particle (virion) consists of a DNA core (green) surrounded by an icosahedral capsid (white), which is itself surrounded by an envelope covered in glycoprotein spikes (green outline). AMI Images/Science Photo Library, Computer artwork of an HSV particle. Russell Kightley/Science Photo Library, Section through a nerve ganglion showing clusters of nerve cell bodies. Microscape/Science Photo Library. Illustrations by James B. W. Ilustration..
