HIV and the ‘functional’ cure
Issue: Sexually transmitted infections (STIs)
21 May 2013 article
Earlier this year there was much media coverage surrounding news that doctors in the US had ‘functionally cured’ a baby born with HIV, who now no longer needs medication for the disease. Here’s a short background explaining the case.
BEN THOMPSON
The results of this case were presented by researchers at the 20th Conference on Retroviruses and Opportunistic Infections in March 2013. They described the case of an unnamed child born in Mississippi State to a mother who was unaware of her HIV status until she was tested during labour and found to be positive. Doctors began treating the baby 30 hours after the birth with a cocktail of three antiretroviral drugs, a different treatment regime from the one or two drugs usually given to prevent mother-to-child transmission after birth.
While initial tests showed the child to be HIV-positive, 1 month on the three-drug therapy caused the virus levels in the blood to drop to undetectable levels. The baby remained on the therapy for 18 months before treatment ceased for approximately 5 months. Normally, a break in treatment causes levels of HIV to bounce back to detectable levels. In this case, much to the surprise of the clinicians, the child’s virus levels remained undetectable, although traces of viral genes were detectable.
Prolonged, timely therapy can lead to a functional cure; however, it clearly doesn’t work for everyone.
This is where the word ‘functional’ in functional cure becomes important; while viral genes were detected, it appears that the child need never take antiretroviral drugs again and is unlikely to be infectious to others. This is clearly a remarkable discovery but currently no one knows how, or why, it occurred. The science is yet to be published in a peer-reviewed journal and it is important to note that n=1.
The circumstances surrounding this case are unusual too. Had the mother known she was HIV- positive, an appropriate treatment regime would have lessened the chances of her having an infected child. The UK Health Protection Agency reported that routine antenatal screening meant that 99% of the babies born to women diagnosed as HIV-positive in the UK between 2006 and 2010 were not infected with HIV.
Around the same time, in a study published in PLOS Pathogens, French researchers demonstrated another functional cure, this time in a group of patients who were part of a ‘Viro-Immunological Sustained CONtrol after Treatment Interruption’ (VISCONTI) study. Fourteen members of the study (out of a total of 70) who received a standard HIV antiretroviral combination within the first two months of being infected maintained low or undetectable virus levels several years after this long-term drug therapy (www.plospathogens.org/article/info%3Adoi%2F10.1371%2Fjournal.ppat.1003211).
As before, this is clearly an important result and shows that prolonged, timely therapy can lead to a functional cure; however, it clearly doesn’t work for everyone. The science that underpins why certain patients maintain these low or undetectable levels of virus after therapeutic treatment remains unreported. It is potentially of use in sub-Saharan Africa, which saw approximately 1.8 million new infections in 2009, but is a tantalising possibility that remains some way off. This treatment regime (www.unaids.org/globalreport/documents/20101123_GlobalReport_full_en.pdf) requires rapid diagnosis and treatment, which is unavailable to many in this region.
Until these findings produce meaningful clinical applications – and this could take years, if not decades –
ensuring that people have access to education, condoms, screening and affordable, effective treatment remains the best way of tackling this disease.
BEN THOMPSON
Senior Public Relations Officer, SGM;
Email [email protected]
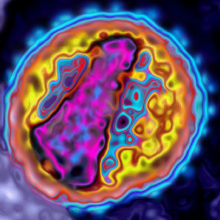
Image: False-coloured transmission electron micrograph of ahuman immunodeficiency virus (HIV) particle, the retrovirus that causes acquired immune deficiency syndrome (AIDS). James Cavallini / Science Photo Library.
