From zero to zero in 100 years: gonococcal antimicrobial resistance
Issue: The Mobile Microbe
08 November 2016 article
The threat of antimicrobial resistance (AMR) in bacteria has been escalated to a rightful seat on the global health agenda. In September 2016, for only the fourth time in United Nations (UN) history, the UN General Assembly in New York will meet to focus on a health threat – antimicrobial resistance. Other diseases afforded this level of consultation at the UN were human immunodeficiency virus (HIV), non- communicable diseases and Ebola virus. There are grim predictions for the future in terms of AMR and health security that span income settings. These predictions challenge the premise that minor bacterial infections of childhood are innocuous, and threaten to halt the medical advancements dependant on antibiotic therapy. Those with compromised immune systems, whether endogenous or induced, will be at highest risk. The development and spread of AMR has been, and will continue to be, fanned by the relentless selection pressure of exposure to antibiotics whether used appropriately, unnecessarily or suboptimally, in human health, animal health and agriculture. The distribution of antibiotic resistant bacteria is facilitated by travel and transport. Antimicrobial resistance will affect those in the community and the hospital.
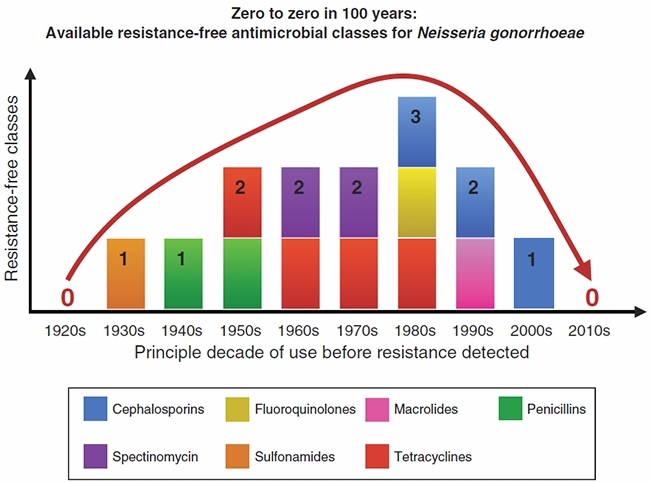
A well-documented example that demonstrates the development and spread of AMR involves Neisseria gonorrhoeae (Figure 1). The expansion of AMR to each successive therapeutic recommendation has left limited options for treatment of this once easy-to-treat infection. International travel remains a major factor in the dissemination of drug-resistant Neisseria gonorrhoeae strains and this has been highlighted most recently by the global spread of strains with resistance to extended spectrum cephalosporin antibiotics, the so-called last single dose therapy. Now a combination of two antibiotics are generally recommended for the treatment of gonorrhoea, ceftriaxone and azithromycin, and resistance to both has been documented1,2. Resistance to azithromycin is typically caused by alteration of the 23S ribosomal RNA gene (the drug target), but may also arise via mutations causing increased activity of efflux pumps (which pump drugs out of the cell)3. Resistance to cephalosporin antibiotics is characterised by a mosaic penicillin binding protein-2 (PBP-2) (this mosaic PBP-2 occurs as a result of integration of DNA sequences from other bacteria producing a changed drug target). Mosaic PBP-2 strains belonging to multi-locus sequence type 1901, first reported in Japan at the turn of the millennium, have become a successful clone in several continents. Whilst genetic data are lacking to confirm what happened with the previous first-line antibiotic classes, it is likely that a similar global transmission event was responsible for limiting the use of fluoroquinolones in the early 1990s.
FIGURE 1. GONOCOCCAL ANTIMICROBIAL RESISTANCE OVER THE PAST 100 YEARS. BARS INDICATE THE NUMBER OF CLINICALLY TESTED ANTIMICROBIAL CLASSES AVAILABLE FOR NEISSERIA GONORRHOEAE TREATMENT.
Many questions remain regarding how to best deal with AMR in Neisseria gonorrhoeae. A gonococcal vaccine remains elusive and other primary prevention strategies, such as safer sex behaviour change strategies have not prevented the spread of gonococcal AMR. Many regions of the world remain unaware (particularly at the population level) of the nature and extent of gonorrhoea prevalence and the incidence of antimicrobial resistance. In addition, international travel continues to threaten AMR containment and border screening is not a realistic option for preventing spread of AMR. For these reasons, ongoing monitoring of AMR, both at national and global levels, remains the central tenet of the public health response to the threat of untreatable gonorrhoea. In our opinion, this can only be achieved through combined use of both bacterial culture and molecular AMR testing strategies. Culture based surveillance remains optimal for detecting new resistance mechanisms. However, mechanism and strain-specific molecular assays add rapid, important and clinically relevant data for situational analysis and to inform treatment guidelines, to monitor the effect of interventions and to provide data in countries or remote areas with limited laboratory capacity.
Gonococcal diagnostic and AMR testing strategies in remote and regional communities of Australia provide an ideal fine scale example of the above. These communities represent one of the few globally where penicillin can still be used for treatment of locally acquired gonorrhoea. Penicillin is an ideal treatment option as it is orally administered, and can be stored without need for refrigeration hence there is considerable motivation to maintain this therapeutic option. Incursion of penicillin resistant strains from elsewhere in Australia, where resistance rates exceed 40%, or from international travellers, is an ever-present threat. Optimal surveillance is pivotal to identify such incursions and initiate rapid public health interventions. Whilst gonococcal culture is promoted, the majority of infections (~90%) are diagnosed by molecular based testing. To facilitate surveillance locally, an in-house polymerase chain reaction (PCR) assay has been developed and implemented to screen for penicillinase-producing Neisseria gonorrhoeae (PPNG) strains. This approach has a key benefit: rather than simply responding to emerging trends in aggregate data, the assay provides immediate results at an individual level that can readily be acted upon.
The recent incursion of the ceftriaxone resistant A8806 strain into Australia exemplifies how the dual culture-molecular approach supports public health initiatives to contain gonococcal AMR4. The A8806 isolate was first identified by culture (highlighting the importance of maintaining bacterial culture). After the phenotypic AMR profile was established using conventional culture-based techniques, the isolate was sequenced, and a strain-specific PCR method developed. The PCR was utilised in clinical practice to determine the spread and prevalence of the A8806 strain across the two states where the infected patient had travelled. We are currently investigating an outbreak of azithromycin resistance in Australia, and further intend to use molecular assays to gauge the extent of the outbreak. Increasingly the availability of genome sequencing is facilitating the identification and characterisation of such clusters, permitting tracking and tracing of AMR strains and investigation of transmission dynamics.
The WHO’s Report on global sexually transmitted infection surveillance 2015 shows that in many regions where disease rates are high there is limited data to determine the scope and extent of AMR5. This is a function of a number of factors including limited resources and syndromic management of patients. Paradoxically, best resourced settings often test relatively few gonococcal isolates for AMR, due to a preference for nucleic acid tests which do not characterise AMR profiles of well documented resistance genes. Gonococcal antimicrobial susceptibility testing remains expensive and technically difficult. Strategies are required to strengthen local laboratory capacity and capability, to increase the number of isolates for testing, with all options available to gather timely and reliable information considered.
A population-based approach that identifies those at risk for gonococcal infections, possibly linked to other health interventions, such as HIV screening of high risk people, may be reasonable. Containing gonococcal AMR should be program oriented, linking patient and contact management with the best treatments to prevent disease and reduce transmission. Merging cutting edge molecular technologies that can diagnose known and emerging AMR determinants with new ways of case finding, and bringing effective treatment to patients and partners in a timely fashion will improve health outcomes. Thus a strategy that focusses only on the acquisition of AMR data and which is isolated from other components of an active program to ensure treatment and elimination of transmission is bound to fail. Such programs may entail a shift in thinking regarding how AMR is diagnosed, how and what patients are identified, and the criteria for which treatment guidelines are modified.
Critically N. gonorrhoeae infects only humans and can therefore be potentially eradicated. Future success in the current context will rely on adaptive thinking, exploiting both new and pre-existing technologies to gather information and inform health care strategies. However, primary prevention must remain the principle focus.
MONICA M. LAHRA
WHO Collaborating Centre for Sexually Transmitted Diseases, Sydney, Department of Microbiology, South Eastern Area Laboratory Services, Prince of Wales Hospital, Randwick, NSW 2031, Australia
School of Medical Sciences, Faculty of Medicine, The University of New South Wales, Kensington, NSW 2033, Australia
[email protected]
JO-ANNE R. DILLON
Department of Microbiology and Immunology, College of Medicine, University of Saskatchewan, Saskatoon, Saskatchewan, Canada
C.R. ROBERT GEORGE
WHO Collaborating Centre for Sexually Transmitted Diseases, Sydney, Department of Microbiology, South Eastern Area Laboratory Services, Prince of Wales Hospital, Randwick, NSW 2031, Australia
DAVID A. LEWIS
Western Sydney Sexual Health Centre, Parramatta, NSW 2150, Australia
Marie Bashir Institute for Infectious Diseases and Biosecurity and Sydney Medical School-Westmead, University of Sydney, NSW 2006, Australia
TEODORA E. WI
Department of Reproductive Health and Research, World Health Organization, Geneva Switzerland
DAVID M. WHILEY
Pathology Queensland Central Laboratory, Brisbane, Qld 4029, Australia
The University of Queensland Centre for Clinical Research, Royal Brisbane and Women’s Hospital Campus, Herston, Qld 4029, Australia
REFERENCES
- World Health Organization (2016) WHO Guidelines for the Treatment of Neisseria gonorrhoeae. World Health Organization, Geneva.
- Fifer, H. et al. (2016) Failure of dual antimicrobial therapy in treatment of gonorrhea. N. Engl. J. Med. 374, 2504–2506. doi:10.1056/NEJMc1512757
- Goire, N. et al. (2014) Molecular approaches to enhance surveillance of gonococcal antimicrobial resistance. Nat. Rev. Microbiol. 12, 223–229. doi:10.1038/nrmicro3217
- Lahra, M.M. et al. (2014) A new multidrug-resistant strain of Neisseria gonorrhoeae in Australia. N. Engl. J. Med. 371, 1850–1851. doi:10.1056/ NEJMc1408109
- World Health Organization (2016) Report on global sexually transmitted infection surveillance 2015. World Health Organization, Geneva.
Image: Figure 1. Monica M. Lahra, Jo-Anne R. Dillon, C.R. Robert George, David A. Lewis, Teodora E. Wi and David M. Whiley..
