Global surveillance & response to the threat posed by infectious diseases
Issue: The Mobile Microbe
08 November 2016 article

The international spread of infectious disease has long been recognised. As early as the 14th century, even though the microbial aetiology of communicable diseases was not understood, international travellers were kept in quarantine to prevent the spread of diseases such as the plague. In modern times, the ready availability of international air travel and other forms of rapid transport has made containing the spread of disease even more of a challenge.
To this end, International Health Regulations (IHR) were developed by the World Health Organization (WHO) in 1969 to enable countries to work together to prevent and control public health threats while at the same time trying to avoid unnecessary interference with international travel and trade. The IHR have their origin in the International Sanitary Regulations, originally devised in Paris in the mid-19th century in response to the need for international cooperation in public health following the cholera epidemics that hit Europe in 1830 and 1847.
The importance of surveillance
The development of interventions to control the spread of infectious diseases requires an understanding of their underlying epidemiology. The cornerstone of epidemiology is surveillance, which comprises the collection, collation and analysis of data on the occurrence and burden of disease and the dissemination of information to those who need to know; this will include public health officials, policy-makers, healthcare professionals and the public. While many countries, at least in high-income economies, have national surveillance systems, global surveillance coupled with action to control disease spread is much more complex, requiring international cooperation and sharing of information. As an example of this, Public Health England has published its Global Health Strategy (2014–2019) as part of its commitment to improving health globally. At a wider geographical level, the European Centre for Disease Prevention and Control (ECDC) coordinates a number of pan-European surveillance networks for a range of diseases (Table 1), with responsibility for provision of national data resting with competent bodies in each country. For surveillance of antibiotic resistance, a further network known as CAESAR (Central Asian and Eastern European Surveillance of Antimicrobial Resistance), established by the WHO Regional Office for Europe, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the Dutch National Institute for Public Health and the Environment (RIVM) includes all countries of the WHO European Region that are not part of the European Antimicrobial Resistance Surveillance Network (EARS-Net).
TABLE 1. SURVEILLANCE NETWORKS MANAGED BY THE EUROPEAN CENTRE FOR DISEASE CONTROL COVERING A RANGE OF INFECTIONS
|
Disease area |
Networks |
|
Antimicrobial resistance and healthcare-associated infections |
|
|
Emerging and vector-borne diseases |
|
|
Food- and waterborne diseases and zoonoses |
|
|
HIV, STI and blood-borne viruses |
|
|
Influenza and other respiratory viruses |
|
|
Tuberculosis |
|
|
Vaccine-preventable diseases and invasive bacterial infections |
|
In 1995, a resolution was submitted to the World Health Assembly, urging all WHO Member States (MS) to strengthen surveillance and reporting of re-emerging and new infectious diseases. In response, the WHO created a global surveillance system comprising a ‘network of networks’ which link together existing local, regional, national and international networks of laboratories and medical centres into a super surveillance network. Participants include the WHO Collaborating Centres and Regional Offices, national and international public health bodies and centres of excellence such as the ECDC, the US Centers for Disease Control and Prevention (CDC), reporting networks of UN agencies (e.g. UNICEF) and the Training in Epidemiology and Public Health Intervention Network (TEPHINET), which provides field epidemiology training programmes in 88 countries. Other participants include non-governmental organisations such as the Red Cross, the Red Crescent, Médecins Sans Frontières and Medical Emergency Relief International (Merlin).
Following the epidemic of severe acute respiratory syndrome (SARS) in 2003, the IHR were revised in 2005 to further strengthen surveillance and response capability. The revised IHR (2005), which are legally binding, came into force in July 2007, and represent an agreement between 196 countries, including 194 WHO MS, to build capacity to detect, assess and report public health threats in a timely manner. There is also a requirement to ensure that international ports, airports and ground crossings have the capacity to deal with public health threats and limit the spread of disease into neighbouring countries. However, in practice such activities are very resource-intensive, and in 2015, only 43% of participating countries reported having achieved full compliance.
Sharing information via the Internet
In addition to the formal surveillance activities described above, a vast amount of data is now collected and shared using the Internet, with freely available electronic discussion sites being valuable sources of information. This is particularly important for the collection of information from low-income countries, which often lack robust surveillance systems due to lack of resources and poor national infrastructure. The scope of this approach may be worldwide [e.g. ProMed (Program for Monitoring Emerging Diseases)], regional (e.g. PACNET in the Pacific region) or national (e.g. Sentiweb in France). This approach to information gathering is being increasingly used by healthcare professionals, an example being the Global Public Health Information Network (GPHIN), an electronic surveillance system developed by Health Canada which has search engines that actively trawl the Internet for reports of communicable diseases in electronic discussion groups or on news wires. GPHIN has begun to search in English and French and will eventually expand to all official languages of the WHO. Another such system is HealthMap, developed by a team at Boston Children’s Hospital in 2006. Data on emerging public health threats are made freely available via the Internet at www.healthmap.org/en and are also available from the mobile app, Outbreaks Near Me. The aggregated data provided by HealthMap are derived from a wide range of freely available sources including, among others, ProMED, GeoSentinel (clinician-based sentinel surveillance of individual travellers), OIE (the World Organization for Animal Health [Office International des Epizooties]), FAO (Food and Agriculture Organization of the UN), Eurosurveillance and Google News. It is of note that in early 2014, HealthMap tracked early press and social media reports of a haemorrhagic fever in West Africa that was subsequently identified by WHO as Ebola.
The global response to disease
Public health threats posed by some disease outbreaks may extend beyond an affected state’s national border and require coordinated international action. After convening an expert Emergency Committee, WHO may designate these as Public Health Emergencies of International Concern (PHEICs), allowing the implementation of temporary control measures. WHO may also coordinate a response using resources from the Global Outbreak Alert and Response Network (GOARN), which is a collaboration of existing institutions and networks in different countries. A WHO team may be sent to instigate initial control measures and make an assessment of the response required. Rapid dissemination of information is important, and WHO alerts are made publically available via the Internet at www.who.int/csr/don/en.
Re-emerging and new infectious disease threats
Despite advances in medicine, public health continues to be threatened by re-emergence and international spread of infectious diseases thought to have previously been under control such as tuberculosis (TB), which is now increasingly difficult to treat due to multidrug resistance (Fig. 1). In addition, recent decades have seen the emergence of new infectious agents such as severe acute respiratory syndrome (SARS), Middle East respiratory syndrome coronavirus (MERS-CoV) (Fig. 2), Ebola, Zika virus and chikungunya, as well as new variants of known pathogens such as influenza virus. We have also seen the emergence of new syndromes such as microcephaly associated with the Zika virus (Fig. 3) and hantavirus pulmonary syndrome. Efforts to control the spread of these infections will require improved detection, diagnosis and reporting, as well as close international collaboration and sharing of information to trigger international responses. These will include mobilisation of healthcare personnel, and provision of clinical and travel advice aimed at mitigating the spread of disease.
FIG. 1. CASES OF MULTIDRUG-RESISTANT TB IN EUROPE IN 2014.
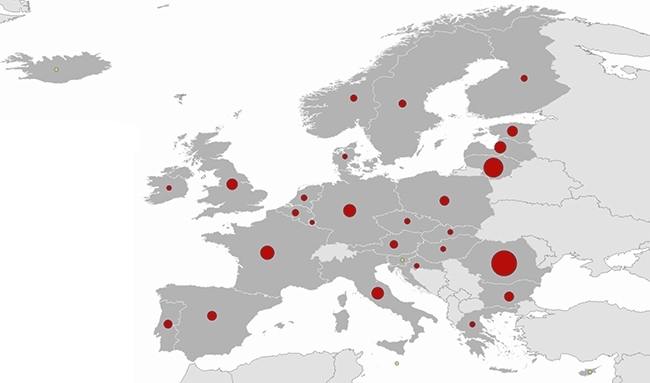
FIG. 2. TIME TREND FOR CONFIRMED GLOBAL CASES OF MERS-COV REPORTED TO WHO AS OF 22 JULY 2016 (N=1791).
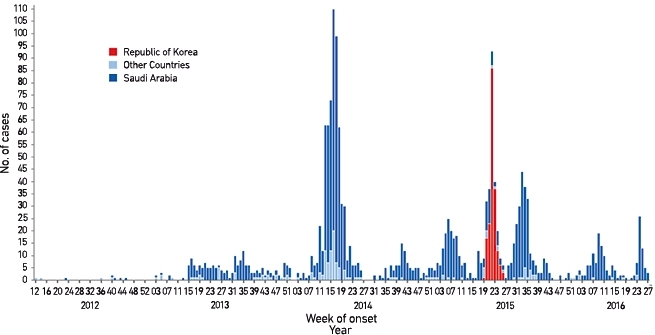
FIG. 3. GLOBAL OCCURRENCE OF ZIKA VIRUS REPORTED VIA HEALTHMAP FOR THE LAST WEEK OF JULY 2016.

ALAN P. JOHNSON
Department of Healthcare-Associated Infection & Antimicrobial Resistance, National Infection Service, Public Health England, London NW9 5EQ, UK
[email protected]
JOANNE FREEDMAN
Travel and Migrant Health Section, National Infection Service, Public Health England, London NW9 5EQ, UK
[email protected]
FURTHER READING
European Centre for Disease Prevention and Control. Public health and disease networks. Accessed 22 August 2016.
Public Health England. Global Health Strategy, 2014 to 2019. Accessed 22 August 2016.
St Louis, M. (2012). Global health surveillance. Morbidity and Mortality Weekly Report. 61(03), 15–19.
World Health Organization (2005). International Health Regulations, Second Edition. Accessed 22 August 2016.
WHO Regional Office for Europe. Central Asian and Eastern European Surveillance of Antimicrobial Resistance (CAESAR). Accessed 22 August 2016.
Image: Plane at sunset. Thinkstock. Fig. 1. Dataset provided by ECDC based on data provided by WHO and Ministries of Health from the affected countries (data available here). Fig. 2. WHO. Fig. 3. HealthMap..
