A (brain) slice of the Rift Valley fever virus puzzle
My name is Kaleigh Connors, and I am a 4th year doctoral candidate in the lab of Amy Hartman at the University of Pittsburgh Center for Vaccine Research, USA. The Hartman lab studies emerging zoonotic viruses, including Rift Valley fever virus (RVFV), to better understand disease pathogenesis. The goal is to translate our basic pathogenesis work to the applied evaluation of vaccines and therapeutics.

Our latest study focused on the development and characterization of an ex vivo rat brain slice culture model to study Rift Valley fever (RVF) neuropathogenesis. RVFV is a mosquito-borne virus currently endemic to the African continent and parts of the Middle East. Since its discovery in the 1930s, outbreaks have occurred regularly in both livestock and people. While much disease in humans is asymptomatic or self-limiting, a proportion of people may develop more severe outcomes, which includes hepatitis, hemorrhagic fever, vertical transmission and encephalitis. Despite the potential to cause these severe outcomes in humans, RVFV remains understudied.
One of the main reasons why neurologic disease is an understudied outcome is that it is difficult to model RVF neurologic disease in a laboratory setting. Traditional rodent models, such as mice and rats, exhibit inconsistent outcomes when infected with RVFV. Most inbred mouse strains develop lethal hepatic disease shortly after infection, while rats succumb to hepatitis or develop asymptomatic disease. However, our lab identified that aerosol exposure of certain rat strains to RVFV consistently induces neurological symptoms, such as tremors and paralysis, before the animals succumb to the disease. While this model has proven invaluable, its practicality is hindered by the high cost, time, expertise and equipment required for aerosol exposure, thus limiting its widespread use.
We developed an ex vivo rat brain slice culture system to complement our in vitro and in vivo models for studying RVFV infection. This method preserves the natural cytoarchitecture and cellular interactions of brain tissue, unlike primary cell cultures. Ex vivo brain slices encompass all relevant cell types and functions observed in vivo, simplifying experimentation compared to live animal studies. This approach, previously utilised in studying other neurotropic viruses, offers a promising avenuw for investigating RVF neuropathogenesis and testing potential therapeutics.
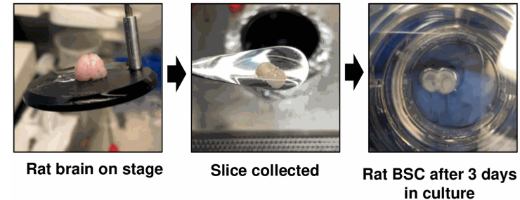
The first step of using this model to study RVFV was to get the ex vivo brain slices working in our hands. Several other groups have published protocols which were adapted to generate the method described in our paper. We found that isolation of 400 uM thick coronal slices from postnatal day 6 rats yielded viable tissue through two weeks in culture. By using both a lactate dehydrogenase (LDH) release assay and a measure of metabolic activity (MTT assay), we observed continued integrity of the slices up to 13 days in culture. This extended timeline in culture allowed us to by-pass an initial post-slice inflammatory response that could antagonise viral infection. We opted to infect our brain slices at 10 days in culture.
The most exciting part of this work was confirmation that ex vivo brain slices were viable after slicing and culture, meaning they were ready for infection! We infected slices with three inoculation doses of wildtype RVFV strain ZH501. Using both viral RNA quantification and viral plaque assay (VPA), we show that ex vivo rat brain slices are permissive to infection by RVFV and support viral replication in a dose-dependent manner. At the highest input dose, virus replicates to up to 1 x 107 pfu equivalents per ml.
Another exciting aspect of this work is the ability to use confocal immunofluorescent microscopy to observe cellular changes and viral pathogenesis over time. We and others have shown that many cells within the brain are permissive to infection by RVFV, including neurons, astrocytes and microglia. After using a quick clearing method for brain slices, we used immunofluorescent microscopy to observe direct infection of neurons through co-localisation of viral antigen and neuronal markers NeuN or Beta III tubulin. In addition, we identified morphological changes in IBA-1 expressing (microglia) and GFAP expressing (astrocyte) cells, suggesting they became activated during infection. This finding was particularly interesting as we were able to capture these responses across several slices and visualise how viral infection impacted the entire tissue microenvironment.
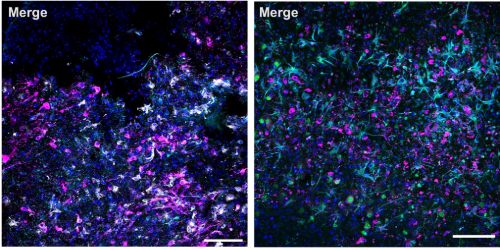
Activated microglia and astrocytes increase expression of inflammatory cytokines and chemokines. In fact, we showed that an antiviral response to infection is maintained in the ex vivo slice cultures through the quantification of changes in gene expression of chemokines and cytokines. We show an increase in antiviral markers IL-6, GRO/KC, MCP-1, IL-18, IL-1b, TNFa and interferons, through 72 hours of infection. The ex vivo model allows us to directly assess the response of resident brain cells to RVFV infection.
It was recently shown that following infection with RVFV, a viral non-structural protein called NSs interacts with apoptotic protein active caspase-3 in the nuclei of infected cells. Using an LDH assay, we demonstrate that rat brain slices infected with RVFV produce higher amounts of LDH compared with mock-infected slices. This suggests that RVFV infection of the slices induces tissue damage. Further, when we used immunofluorescent microscopy to observe activation of apoptosis, we imaged active caspase-3 as filamentous structures in the nuclei of RVFV infected cells. This indicates that RVFV infection of ex vivo rat brain slices may serve as a complementary tool to study host-virus interactions.
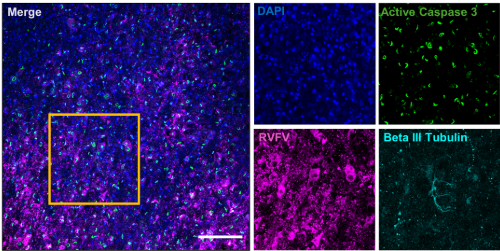
Image of ex vivo rat brain slice during RVFV infection (48 h p.i.). Cell nuclei in blue. RVFV-N in pink. Neurons in cyan. Active caspase 3 in green.
We hope to continue to utilise these ex vivo brain slices to better understand the neuropathogenesis of RVFV. Our next step is to utilise ex vivo rat brain slices to assess antivirals and therapeutics prior to in vivo testing. In addition, we aim to expand upon the imaging capabilities of ex vivo slices to interrogate the role of glia and other resident brain cells during RVFV infection.
Image: Kaleigh Connors
