A new player in Pseudomonas aeruginosa biofilm regulation
Posted on September 5, 2012 by Sarah Maddocks, Cardiff Metropolitan University
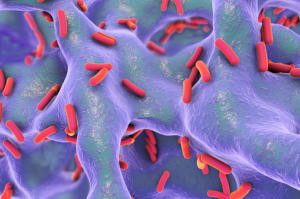
Pseudomonas aeruginosa is a human pathogen commonly associated with lung infections in cystic fibrosis sufferers, and is emerging as the most prevalent cause of infection in burns patients. Multidrug-resistant strains of P. aeruginosa make this micro-organism difficult to treat – a problem that is exacerbated by its tendency to live in communities known as biofilms.
A novel transcriptional regulator, PyeR, has been identified and characterized as a major player in P. aeruginosa biofilm formation, as reported in Microbiology.
The research identifies PyeR as a member of a super-family of transcriptional regulators, ArsR, that are involved in the bacterial response to metals such as nickel, copper, cadmium and zinc. These regulators control the transport of metal ions in and out of bacterial cells. PyeR, on the other hand, is thought to have quite a different function, primarily involved in biofilm formation, and has been classified in a sub-group of the ArsR family involved in varying physiological functions aside from metal ion transport. This is only the second report that has implicated any member of the ArsR family in the regulation of biofilm formation.
The synthesis of PyeR is intricately controlled, and may form part of a wider regulatory network governing the expression of antibiotic resistance traits, virulence factors and biofilm formation. When PyeR is absent there are no changes in the resistance of P. aeruginosa to antibiotics and no change in its virulence. However, biofilm growth is significantly altered suggesting a role for PyeR in biofilm regulation.
It is becoming increasingly evident that for many bacteria, the biofilm lifestyle is the norm. Biofilms are renowned for their resilience to antimicrobial treatment; for bacteria of medical significance this poses a huge problem in terms of persistent and recurrent infection. Understanding how biofilm development is regulated at the molecular level in a pathogen such as P. aeruginosa will help underpin continuing research into methods of control and treatment. This study opens up new and stimulating avenues for continued exploration into what might trigger the shift towards biofilm growth in P. aeruginosa.

