Comment: The voyages of Zika virus
08 November 2016
The announcement in May this year from the World Health Organization, that the Zika virus outbreak that began in October 2015 in the Cape Verde Islands off the west coast of Africa was an American variant of Zika virus, confirmed that Zika has now circumnavigated the world.
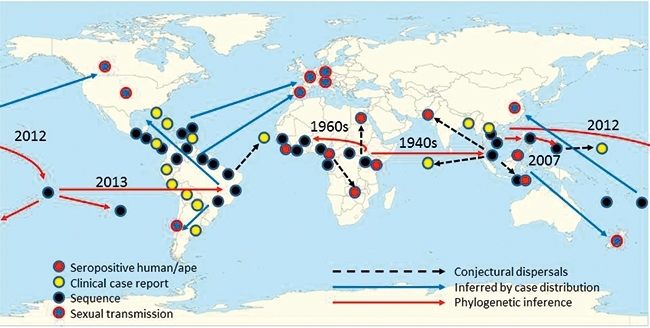
Unlike the first human circumnavigators in the 16th century, who sailed the world from east to west, Zika travelled in the opposite direction, heading east out of Africa to South-east Asia, then across the Pacific Ocean, through the Americas and finally back across the Atlantic to Africa. Zika was discovered by accident in 1947 in macaque monkeys caged in Uganda’s Zika forest as part of a yellow fever monitoring study. A relative of yellow fever in the genus Flavivirus, and spread in much the same way by mosquitoes of the genus Aedes, Zika simply joined the growing list of obscure tropical viruses of no clinical importance, registering barely a dozen mild cases of fever and rash in humans over the next 60 years.
Obscure no more
Then in 2007, the isolated Micronesian island of Yap became the location of the first epidemic in humans. Subsequent serological investigation showed that the majority of the population of a few thousand were infected, and that most of them reported no symptoms. Zika’s potential for disseminated transmission was amply illustrated, but it wasn’t until 2013 that the clinical implications of this became clearer. In that year, an even bigger outbreak occurred in Polynesia, infecting tens of thousands and adding an unwelcome new symptom to Zika’s clinical description – Guillain-Barré syndrome, an auto-immune paralysis. Even then, there were no fatalities, and it wasn’t until Zika completed the trans-Pacific leg of its journey, arriving in Brazil during or before the 2014 World Cup, a wave of foetal microcephaly cases trailing nine months in its wake, that the world finally realised the seriousness of this new pandemic, with the WHO declaring a Public Health Emergency of International Concern (PHEIC) on 1 February 2016.
Out of Africa
Why Zika should suddenly cause so much trouble after decades, perhaps centuries, of obscurity, remains a mystery. We have good grounds to believe that Zika originated in Africa, for the classic population genetic reason – which also applies to human immunodeficiency virus (HIV) and hepatitis C virus (HCV) – that the African strains are more genetically diverse than the non-African ones, indicating an accumulation of variation over a longer period of time. Diversity within the Asian and American strains is comparatively small and Bayesian phylogenetic analyses have dated Zika’s emergence from Africa in the early- to mid-20th century. Zika’s sporadic appearances in Africa have been in a belt from Uganda, through the Central African Republic to Nigeria and Senegal in the west, and its first isolation outside of Africa was in Malaysia in the 1960s. Just as earlier slave trade movements probably exported Zika’s relative yellow fever from Africa across the Atlantic to the Americas, it is easy to imagine later colonial migrations, possibly administrative, commercial or military, carrying Zika from the British colonies in East Africa to those in South-east Asia. The fact that it didn’t reach the Americas along with yellow fever in the 18th century suggests that Zika was rare in West Africa at that time, and indeed we have no up-to-date information on Zika’s incidence in Africa now, except for a handful of serological studies conducted mostly before 1980 which suggest that between 6% and 60% of the African population are exposed to Zika at some point in their lives. In Asia, the corresponding figures are lower: less than 15% at all sites tested, again consistent with a relatively recent arrival from Africa.
Increased virulence or lack of herd immunity?
We cannot currently reconstruct much concerning Zika’s pre-history until we can obtain more genome sequences from both Africa and Asia, and Zika is so far proving a difficult virus to isolate and sequence. A short viraemia and odd compositional content mean that we simply aren’t accumulating genomes as fast as we did with Ebola at the height of the West African outbreak in 2014–15. To a certain extent, however, quality is better than quantity. Most of the Brazilian and other Latin American Zika genomes are very similar, and the really interesting differences are likely to occur away from the leaves of the phylogenetic tree and down in the branches where Asian Zika diversified before setting off across the Pacific. Here is where the crucial genetic differences will be found if it is the case that Pacific/American Zika’s apparently novel properties – wider range of symptoms, possibly a greater transmissibility, Guillain-Barré and microcephaly associations – are due to evolution of the virus. On the other hand, it is perfectly possible that strain differences are inconsequential genetic drift and that what we are really seeing in the Americas is simply yet another example of an introduced pathogen wreaking havoc in a population with no previous exposure. The Native Americans of colonial times suffered terribly from the introduction of smallpox, influenza, yellow fever and even cold viruses from the Old World, and Zika may simply be doing what many viruses tend to do when they enter a host population with no herd immunity.
ZIKA CIRCUMNAVIGATES THE WORLD. THE PATTERN OF SPREAD HAS BEEN DEDUCED FROM PHYLOGENETICS (RED ARROWS), EPIDEMIOLOGY (BLUE ARROWS) OR BY INFORMED GUESSWORK (DOTTED ARROWS).
What now for Africa?
The answer to this question will also have consequences for Africa. The Zika outbreak in the Cape Verde Islands is confirmed by the WHO as being of Brazilian origin, and has been associated with microcephaly. If the islanders have never been exposed to Zika before, we might regard this as a similar situation to Brazil. On the other hand, if African Zika has circulated in Cape Verde, we must wonder why it has not produced a cross-protective effect against the American strain. Meanwhile, Guinea-Bissau has just become the first mainland African country to report an outbreak in recent times. The strain involved is of African origin and not, unlike the strain in Cape Verde, an import from Brazil. What happens there may forewarn us of what might happen elsewhere in Africa. The crucial question is – can African Zika also cause microcephaly? We may soon have an indication from the macaque monkey model of Zika infection used in the vaccine development programme. The current experimental Zika vaccine is based on American strains (Brazilian and Puerto Rican), so if it protects against infection with an African strain, the converse will probably apply and we are unlikely to see a similar epidemic of microcephaly in Africa as we have recently seen across tropical Latin America.
Zika Down Under
Meanwhile, Zika continues to be detected more sporadically in South-east Asia. The lower epidemiological intensity and absence, so far, of microcephaly complications suggests that South-east Asia, perhaps like Africa, has the herd immunity that the Pacific and Americas lack. Since the climate of Indonesia, and also some Aedes mosquito species, is shared by the tropical northern Australian coast, Zika might have been expected to have already arrived in Australia. However, what is different is the absence of a wild monkey species in Australia, which may deprive Zika of the animal reservoir it needs to maintain itself in an area where the human population is mostly immune. In Africa, red-tailed monkeys have been shown to be a Zika reservoir, and in Brazil, Zika has already been detected in marmosets and capuchins. Of course, Australia, like all countries, could also see Zika spread by sexual transmission. This is climate- and mosquito-independent, but we still have no idea if it is sustainable.
DEREK GATHERER
Faculty of Health & Medicine, Lancaster University, Lancaster LA1 4YG
[email protected]
