Phage therapy
09 August 2016
As early as 1945, in his Nobel Prize Lecture titled ‘Penicillin’ Alexander Fleming declared, “There is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant”.
Fleming’s speech was prescient. In May of this year (2016) headlines around the world reported the case of the first known US patient to be infected with Escherichia coli bacteria that possess resistance to a ‘last resort’ antibiotic, colistin. This was not the first time that ominous stories about colistin-resistant bacteria hit the headlines; colistin-resistant bacteria have been found in China, Canada and Europe, including the UK. The implications are clear: we are running out of effective antibiotics as the number of antibiotic-resistant pathogens continues to increase and even the antibiotics of last resort are losing their efficacy.
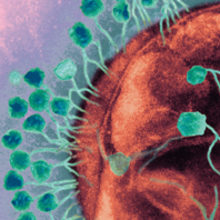
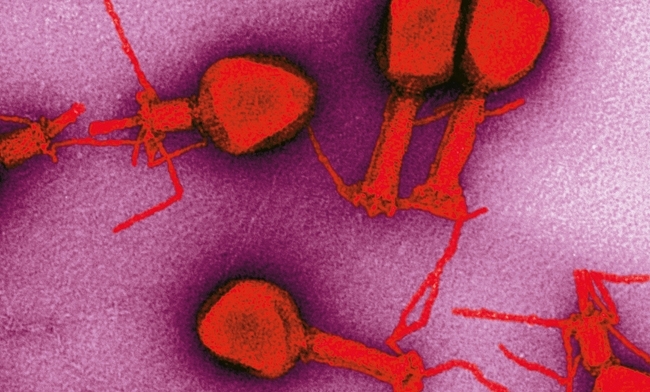
Tackling this growing crisis is an urgent priority and attention is focusing on protecting and preserving the antibiotics that we have at our disposal, as well as hunting for new antimicrobial products. Antibiotics work by targeting and destroying bacteria. However, they are not unique in that respect. Bacteriophages, or phages for short, can also target and destroy bacterial cells. Phages are ubiquitous; they are found in seawater, freshwater, soil and sewage slurries. It is estimated that there are 1030–1032 phages in the biosphere and every 48 h, phages infect and destroy about half the bacteria in the world. The remarkable thing about phages is their specificity to target particular bacterial species.
Phage therapies from the past
In 1915, more than 10 years before Fleming’s article on penicillin, an English doctor called Frederick Twort (1877–1950) published an article entitled ‘The Infectious Disease of the Micrococcus’ in The Lancet. It described how a phage infection of colonies of Staphylococcus gave rise to clear zones of lysis as the phages appeared to destroy the bacteria. In 1917, the French Canadian microbiologist, Félix d’Herelle (1873–1949) described these infectious particles as bacteriophage (as they ‘eat’ bacteria). The name has stuck to this day. In 1919, shortly after the end of the First World War, d’Herelle used phages to treat dysentery for the first time in the Hôpital des Enfants-Malades in Paris. The phage preparation was administered to a 12-year-old boy suffering with severe dysentery. The patient’s symptoms improved immediately and the boy recovered fully within a few days. Encouraged by the success of his original solution, new preparations of bacteriophages were prepared to target other bacteria, including Vibrio cholera and Yersinia pestis. Soon, reports began to emerge that these new phage solutions were successfully treating thousands of people in China, Laos, India, Vietnam and Africa who were suffering from cholera and bubonic plague.
Pharmaceutical companies began to sell phage solutions commercially. D’Herelle’s laboratory in Paris produced phage preparations against various bacterial infections that were sold by what became the large French company L’Oréal. In the 1940s, Eli Lilly and Company (Indianapolis, Indiana, USA) also produced several phage products for human use that targeted pathogens such as staphylococci, streptococci and E. coli. These pathogens are still causing concern today as antibiotic-resistant species continue to increase.
D’Herelle’s collaborations with scientists in Tbilisi, Georgia, ensured that phage therapy was adopted as a clinical treatment for bacterial infection in the former Soviet Union and Eastern Europe. Unfortunately, the results of these studies did not use the rigorous, double-blinded clinical trials that are the current gold standard used to test new therapeutic drugs and interventions today. These studies were extensively published in non-English (primarily Russian, Georgian and Polish) journals. As a result, they were not readily accessible to the western scientific and medical community, and phage therapy rapidly fell out of favour in the west, especially after antibiotics became commercially available.
Phage therapy in the future
However, as there is a dearth of new, clinically relevant antibiotics emerging through the antibiotic discovery pipelines, there is renewed interest in revisiting phage therapy. Currently, there are clinical trials, which are examining the safety and efficacy of phages as topical therapies for treating skin and ear infections in humans, as well as food additives designed to reduce bacterial contamination of ready-to-eat meat, fruit, vegetables and dairy products.
Scientists are exploiting phages in other ways. After phages enter the bacterial cell they force the bacteria to synthesise new phage particles that accumulate inside the cell. At the end of their replication cycle the phages use suicidal enzymes, called endolysins (phage lysins) to degrade the peptidoglycan found in the bacterial cell walls and the progeny phages are released into the environment. The lysis of the bacterial cell is also enabled by another group of phage enzymes, the holins, which are produced during the late stages of phage infection. Holins and endolysins are encoded by the bacteriophage genomes and synthesised by the bacterial cellular machinery. As the holins oligomerise, they punch holes through the inner bacterial membrane. This allows the lysins to move through the cellular membrane to attack and degrade the bacterial cell wall. Phage endolysins differ depending on whether they target the cell wall of Gram-positive or Gram-negative cells. What makes endolysins so interesting is that they can be applied exogenously as recombinant proteins to destroy bacterial cells. In addition, compared with many antibiotics still in clinical use, the endolysins have an added advantage; they exhibit a genus or species specificity. These characteristics offer exciting therapeutic possibilities. Lysins encoded by phages that infect Gram-positive hosts usually contain two distinct domains. They have an N-terminal catalytic domain (CD) and a C-terminal cell-wall binding domain (CBD). Engineering chimeric lysins, or ‘chimeolysins’, by mixing and matching the two domains from various natural lysins offers opportunities for finding novel enzymes with improved properties such as increased solubility and an extended lytic spectrum. Currently, methods for developing chimeolysins, such as domain shuffling, depend largely on a trial-and-error approach, and this limits the efficiency for discovering effective chimeolysins.
Scientific research is currently underway to examine how lysins can be used to treat and destroy pathogens associated with food production such as Clostridium perfringens, which causes necrotic enteritis in poultry and is one of the leading causes of food poisoning in humans. In addition, Staphefekt is the first endolysin to be registered for human use against common skin conditions such as eczema, acne and rosacea, which are caused or exacerbated by Staphylococcus aureus.
Despite the promise of viable antibiotic alternatives and a previous medical history, phage therapy and phage derivatives still provoke serious concerns among the scientific establishment. Issues include the fact that bacteria are just as capable of developing resistance to phages and phage lysins as they are to develop resistance to antibiotics. But phages can also mutate their endolysins and holins, enabling them to re-infect phage-resistant bacteria, and this process happens rapidly and naturally; it does not rely on human intervention. Although humans and animals are constantly exposed to phages, much more research is required to ensure that phages and phage-derived therapy do not cause adverse reactions. As lysins are proteins, they are capable of stimulating an immune response when administered mucosally or systemically. This immune response can potentially decrease the lysis activity. It is absolutely essential that the phages or phage derivatives, such as lysins, are screened to make sure that they are safe to use for human and animal consumption.
Lysins offer enormous potential as effective antibacterials in the fight against infectious disease caused by pathogens with multidrug resistance. Antibiotics such as penicillin and cephalosporin inhibit peptidoglycan synthesis, and only dividing cells are lysed. In contrast, lysins destroy the peptidoglycan directly, killing both growing and non-growing cells. And, unlike antibiotics that often kill bacteria indiscriminately, lysins display a high specificity that ensures that the normal commensal microflora is left undisturbed. As bacteriophages are considered the most abundant biological entities on Earth, they are a rich natural source of these enzymes. It is hoped that bioinformatic and proteomic studies will lead to new opportunities for domain swapping, and the production of specifically engineered designer chimeolysins with diverse applications that will be part of the solution to the growing problem of antibiotic resistance.
LAURA BOWATER
The Norwich Medical School, University of East Anglia, Norwich NR4 7TJ, UK
[email protected]
FURTHER READING
Chanishvili, N. (2012). Phage Therapy – History from Twort and d’Herelle Through Soviet Experience to Current Approaches. Advances in Virus Research, pp. 3–40. Elsevier.
Fenton, M. & others (2010). Recombinant bacteriophage lysins as antibacterials. Bioeng Bugs 1, 9–16.
Stern, A. & Sorek, R. (2011). The phage–host arms race: shaping the evolution of microbes. BioEssays News Rev Mol Cell Dev Biol 33, 43–51.
Twort, F. W. (1925). The Discovery of the “Bacteriophage.” The Lancet 205, 845.
