From NICU to Data-Driven Discoveries: Decoding the Preterm Gut Microbiome
I’m Lauren Beck, a postdoctoral research associate working in the gut microbiome field. I’m based at Newcastle University UK, where I work on a range of projects exploring gastrointestinal health - from early life to adults living with inflammatory bowel disease.
This blog post takes you behind the scenes of a project I started during my PhD a couple of years ago, under the supervision of Professor Chris Stewart, who I continue to work closely alongside. The focus of the study was on one of our most vulnerable population groups: preterm infants born less than 32 weeks of gestation. These babies face a uniquely challenging start to life, especially in comparison to healthy infants born full term. They will initially be cared for on the neonatal intensive care unit (NICU), where they will receive life-saving care, but are also exposed to a number of NICU-specific interventions that can influence how their gut microbiome develops. Factors such as antibiotics, feeding practices, and the hospital environment itself, all play a role in shaping this community. And why does that matter? Because the gut microbiome plays a vital role in human health, and in preterm babies, disruptions to its development have been linked to serious conditions such as necrotising enterocolitis (NEC), a life-threatening gut disease.
In this study, we wanted to understand how different clinical and dietary factors might influence both the gut microbiome (who’s there) and the metabolome (what they’re doing). We were especially curious about how these two systems interacted and evolved over the first weeks of life. To do this, we analysed longitudinal stool microbiome data from 66 infants (266 samples) and metabolomic data from a subset of 55 infants (101 samples). These babies were part of a randomised controlled trial, all on an exclusively human milk-based diet. The original microbiome data has already been published (Embleton et al., 2023) and focused on clinical outcomes. Building on that work, we integrated metabolomics, bringing new insight into not just who is there, but what they’re doing.
As expected, both the microbiome and metabolome changed significantly with age, and infants showed different microbial developmental trajectories, with each infant’s gut community following its own journey. More interestingly, these two layers were intimately linked, suggesting that the microbiome and metabolome develop together during early life. We dug deeper into this complex relationship using microbial—metabolite networks that captured the dynamic interplay between specific bacteria and the chemical compounds they are associated with. Lactobacillus, a commonly known ‘beneficial’ gut bacteria, stood out with the highest number of associations, including equol sulfate, which is related to estrogen metabolism. Together, these patterns offer new insight into how early life exposures shape the developing gut ecosystem in preterm babies.
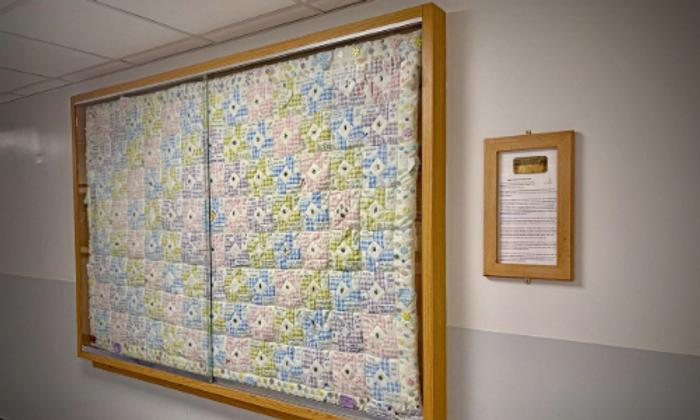
Working with such a fragile patient population means that conducting these kinds of studies is a highly collaborative effort, relying on the incredible support of neonatal teams and families. From collecting and storing samples, to processing in the lab, to data analysis — it takes a coordinated effort across all teams to make a study like this possible. My role is firmly on the data side, and I spend a lot of time buried in code trying to pull everything together. It’s easy to get lost in data, but working on a project like this is a valuable reminder that behind every sample is a real baby, a family, and a clinical question that matters.
Looking ahead, I hope this paper can be a useful resource for other microbiologists and researchers working in the area. The integration of microbiome and metabolome data in this context opens the door for others to revisit these datasets in the future and test new hypotheses, potentially validating their findings in our cohort. We hope this work adds to the growing evidence that clinical and dietary decisions in early life can have measurable effects on gut development and infant health.
Ultimately, our goal is to improve outcomes for preterm babies and their families, not just in the early days, but in the longer term too. It’s an exciting time in microbiome research, but with much more to learn.
