Herpex Simplex Virus 1 and Alzheimer’s Disease
Posted on November 13, 2020 by Professor Ruth Itzhaki
In this blog, Professor Ruth Itzhaki discusses her research into the virus that causes cold sores – Herpes simplex virus type 1 (HSV1). Professor Itzhaki has been investigating the possible links between HSV1 and Alzheimer’s disease for many years. Early in her career, many of her findings were widely rejected by the scientific community, leading to challenges in funding and delays to important research.
Alzheimer’s disease (AD) accounts for about 60% of dementia cases, which affect over 50 million people worldwide. The emotional costs to the patient and carer are huge, and the economic cost associated with the disease is estimated at one trillion US dollars worldwide. These costs will increase with increasing life expectancy, and so it is imperative that effective treatments for AD are found very soon. My lab’s research has implicated a common virus, Herpes simplex virus 1 (HSV1), in the development of AD. This is the first cause of the disease to be proposed, and we suggest that treatment with antiviral agents would slow or even stop disease progression.
The neuropathological features of AD brains are abnormal protein deposits from amyloid plaques and neurofibrillary tangles (NFT). The main components of these plaques are β‐amyloid (Aβ) and abnormally phosphorylated tau (P‐tau). The cause of Aβ and P‐tau formation are unknown, but they play an important role in disease progression.
HSV1 is the main cause of cold sores (herpes labialis). By the age of 60 years, about 80% of the population is infected by the virus. It remains in the peripheral nervous system (PNS) in latent forms of life, but during events such as stress or immunosuppression, the virus reactivates. In some 20–40% of those infected with HSV1, it then causes cold sores.
Whether the virus resides in the brain as well as the PNS was unknown until my lab investigated post-mortem brain specimens using PCR to seek viral DNA. We discovered that in many elderly people, HSV1 is indeed present in brain; is the first infectious pathogen to be discovered in the brain and confers a strong risk of AD when in the brains of people with the type 4 allele of the apolipoprotein E gene (APOE-ε4). The likelihood of developing AD is 12 times greater for APOE-ε4 carriers who have HSV1 in the brain, than for those with neither factor. HSV1 prevalence in the brain was much lower in young people and in children. We also discovered that the virus can reactivate in brain, then replicate, perhaps persistently, leading to cumulative damage.
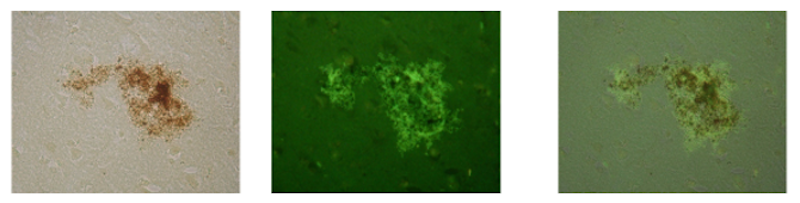
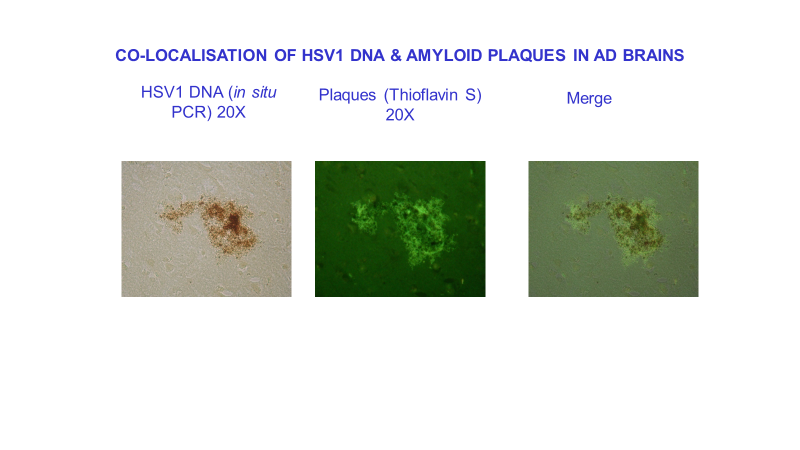
Seeking a link between HSV1 and AD, we discovered that β‐amyloid plaque accumulation occurs in HSV1-infected cells in culture and in brains of HSV1-infected mice. We then showed that in AD brains, most of the viral DNA is located very specifically within these plaques. In normal elderly brains, far less viral DNA is located in plaques, possibly because of lesser production or more efficient removal of β‐amyloid. These results suggest that HSV1 is a cause of toxic amyloid products and plaques. We also found also that the main component of tangles accumulates in HSV1-infected cell cultures.
Following this, we proposed using antiviral agents to treat AD. On treating HSV1-infected cells, an antiviral agent called acyclovir (ACV), or with two other antivirals that target HSV1 DNA replication, we found [9] that Aβ and P-tau do indeed decrease. This is probably through a decrease in viral spread and by inhibiting viral DNA replication. We obtained similar results with other antiviral agents that act in different ways, including intravenous immunoglobulin, and fucoidan, a sulphated polysaccharide which is virucidal and also prevents viral entry into cells.
HSV1 is a major risk factor for AD. The virus enters the brains of older people as the immune system declines and establishes a long-term infection. Events such as stress, immunosuppression or inflammation due to infection can reactivate the virus, leading to damage and further inflammation of the brain. Repeated activation then causes cumulative damage and eventually AD in people with an APOE-ε4 allele. Other studies of ours support the concept that genetic factors can determine the severity of an infectious disease: we have shown that in the case of several diverse microbes, APOE affects outcome of infection. Most relevantly, we discovered that APOE-ε4 is a risk for cold sores; this explains why only some of the many people infected with HSV1 suffer from cold sores. Presumably, in APOE-ε4 carriers, AD develops in brain because of greater HSV1-induced formation of toxic products or lesser repair of damage.
For the first 25 of the last 30 years, this research was virulently opposed – though no scientific objections were ever raised, so, lack of funding and repeated refusals to publish restricted our work and resulted in our surviving (just) on a shoestring. Latterly, we suffered repeated refusals to fund a clinical trial of antivirals. Our results are now supported by about 300 publications from a number of other groups, using very diverse approaches – cell biology, virology, genetics and epidemiology – so the tide is at long last turning. For sure, Alzheimer’s disease will be defeated.
References
Jamieson GA et al. Latent herpes simplex virus type 1 in normal and Alzheimer's disease brains. .J Med. Virol. 33, 224-227 (1991).
Jamieson GAet al. Herpes simplex virus type 1 DNA is present in specific regions of brain from aged people with and without senile dementia of the Alzheimer type. J. Pathol. 167, 365-368 (1992).
Itzhaki RF et al. Herpes simplex virus type 1 in brain and risk of Alzheimer's disease. Lancet 349, 241- 244 (1997)
Lin W et al. Alzheimer’s disease, herpes virus in brain, apolipoprotein E4 and herpes labialis. Alzheimer's Reports 1, 173-178 (1998).
Wozniak MA et al. Productive herpes simplex virus in brain of elderly normal subjects and Alzheimer's disease patients. J. Med. Virol. 75, 300-306 (2005).
Wozniak MA, Itzhaki RF, Shipley SJ, Dobson CB. Herpes simplex virus infection causes cellular beta-amyloid accumulation and secretase upregulation. Neurosci. Lett. 429, 95-100 (2007).
Wozniak MA et al. Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. J. Pathol. 217, 131–138 (2009).
Wozniak MA, et al. Alzheimer's disease-specific tau phosphorylation is induced by herpes simplex virus type 1. J. Alzheimers Dis. 16, 341-350 (2009).
Wozniak MA, Frost AL, Preston CM, Itzhaki RF. Antivirals Reduce the Formation of Key Alzheimer’s Disease Molecules in Cell Cultures Acutely Infected with Herpes Simplex Virus Type 1. PLoS ONE 2011;6(10):e25152. doi: 10.1371/journal.pone.0025152. Epub 2011 Oct 7.
Itzhaki RF. Herpes simplex virus type 1 and Alzheimer’s disease: increasing evidence for a major role of the virus. Frontiers in Aging Neurosci. Aug 11;6:202. doi: 10.3389/fnagi.2014.00202. eCollection 2014 (2014).