How sugar might shape superbugs
Posted on May 9, 2025 by Dr Rebecca J Hall
Dr Rebecca J Hall takes us behind the scenes of their latest publication 'Glucose alters the evolutionary response to gentamicin in uropathogenic Escherichia coli' published in Microbiology.
I’m Dr Rebecca Hall, I’m a Research Fellow at the University of Birmingham (UoB). I’m interested in how microbes evolve, and in my current research with Professor Alan McNally I am looking into the small genetic changes that may prime strains of the global pathogen Escherichia coli to evolve antibiotic resistance.
This paper is part of some work I have been doing independently, investigating how metabolism and the metabolic microenvironment affects bacterial evolution. For this particular project, I had the excellent fortune to work with two really talented students, Shalini Choudhary and Jacob Smith, who were completing their Masters and Undergraduate degrees at the UoB. I also received funding from the University of Birmingham College of Medicine and Health Research Development Fund to support their work.
We were interested in a particular type of E. coli called uropathogenic E. coli, or UPEC. UPEC are the leading cause of urinary tract infections (UTIs), and these infections have large impacts in terms of morbidity and mortality globally. Recurrent UTIs are particularly impactful on an individual’s quality of life. UTIs are treated with a range of different antibiotics depending on factors including whether it has progressed to the kidneys or bloodstream, and whether it is a recurring infection.
The urinary tract is metabolically unusual. UPEC in the urinary tract will be exposed to metabolites, including urea and creatinine, but the exact composition will vary depending on the diet and health of the individual. For example, in individuals with uncontrolled diabetes, including pregnancy-induced diabetes, there is an increased concentration of glucose in the urine.
This means that when a person is treated with antibiotics for a UTI, their bacteria will be exposed to not just the antimicrobial but also to the unique and variable metabolites of the urinary tract. How this might affect infection clearance, or, in the longer term, the evolution of antibiotic resistance, is not yet known.
Here, we focused on how a moderately high concentration of glucose might affect the evolution of UPEC. We used a single UPEC strain taken from a human urine sample. This strain was part of a collection donated to the McNally lab by James R Johnson. We wanted to know whether the genetic changes selected for by the aminoglycoside antibiotic gentamicin would be different when glucose was also present.
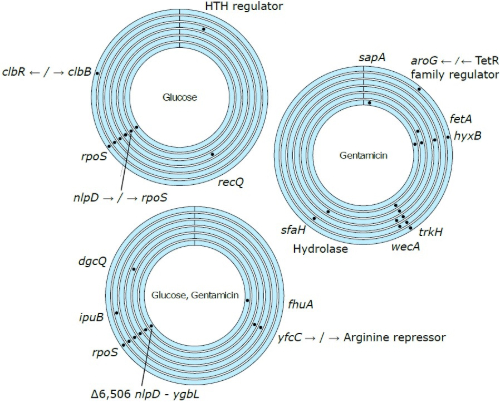
We employed experimental evolution to address our research question. Led by Shalini, we serially passaged individual cultures of UPEC in one of four different conditions: + gentamicin, + glucose, + gentamicin and glucose, and a control line with no added compound. After 21 days of transfers, we selected individual colonies and sent them for short read sequencing with our neighbours at the UoB, microbesNG.
We found several mutations in our antibiotic-exposed populations, including in one gene (trkH) that has already been linked to aminoglycoside resistance. Intriguingly, in the populations exposed to both gentamicin and glucose, we did not find any of these mutations. This suggests to us that glucose might be acting in some way to protect the bacteria from the action of the antibiotic, and as a result altering its evolutionary trajectory.
The exact mechanism behind this remains mysterious, for now. With the expert insight of Professor Jessica Blair, we think that perhaps the glucose is increasing the amount of ATP available, powering efflux pumps to remove gentamicin from the cell. It is also possible that the permeability of the cell is increased in the presence of glucose, reducing the amount of antibiotic that can get in. Watch this space!
A long-term goal of this work is to change how we think about antibiotic prescribing for UTI. Given glucose can be detected in a urine sample quickly and cheaply using a simple dip-stick test, it may be possible in the future to alter the treatment of an individual (e.g. increased dosage) depending on the metabolic composition of their urinary tract, with the overall goal of improving antibiotic efficacy and reducing the likelihood of strains evolving resistance.