CFTR Modulators and Microbial Shifts: Writing a Review as an Undergraduate Researcher
Hello, I am Joshua Robertson, a medical student starting at the Keck School of Medicine of the University of Southern California, USA. I initiated writing this review when I was an undergraduate researcher in the Goldberg Lab at the Emory University School of Medicine Atlanta, Georgia, USA. The Goldberg Lab studies bacteria and how they participate in infections, focusing on the respiratory infections associated with cystic fibrosis (CF). CF is a genetic disorder that causes impaired water balance in epithelial cells, which creates a mucosal environment susceptible to chronic microbial infections associated with morbidity and mortality.
I wrote this review article along with Dr Joanna Goldberg about the impact of cystic fibrosis transmembrane conductance regulator (CFTR) modulator therapies on the pulmonary microbiota. We found a consensus that decreased relative CF pathogen abundance mediated an increase in microbiota diversity. We also identified potential facilitating factors in the literature including direct inhibition, metabolite scarcity, and a decreased inflammatory response. Although more studies to identify the mechanisms and better characterise the longitudinal impacts are needed, the current literature provides promising prospects for the future for people with cystic fibrosis (pwCF).
The idea for this review came up when I was taking a graduate course at Emory University, “Principles of Anti-infectives”. As we discussed and read about the cutting-edge therapies being developed to target microbes and the significant challenges for these therapies like growing antibiotic resistance, I became more interested in ways that bacterial infections are being alleviated by targeting underlying aggravating factors. My research project in the Goldberg Lab at the time was about how Pseudomonas aeruginosa responds to temperature changes, so I started to investigate how P. aeruginosa was being impacted by the change in its environment caused by the widespread adoption of CFTR modulator therapies.
CFTR modulator therapies return function to essential ion channels and bring back water balance. The combination therapy of Elexacaftor, Tezacaftor, and Ivacaftor (ETI) was approved in the US in 2019 and Europe in 2020. ETI therapy, known as Trikafta and Kaftrio commercially, has transformed the lives of pwCF. These therapies have led to improved lung function, increased life expectancy, and a reduction in chronic infection symptoms. Microbiologists like my colleagues in the Goldberg Lab have a particular interest in how these changes impact pathogens. The antibiotic resistance crisis had already displayed how positive innovations can have severe unintended consequences, especially in the dynamic, evolving world of microbes. For these reasons, I was encouraged to write a review about this topic for which the scope quickly expanded to the entire pulmonary microbiota.
Writing a review article was an unfamiliar experience for me. Instead of writing about my own research project, I was synthesising and sometimes critiquing the research of others. Fortunately, writing a review was a part of the “Principles of Anti-infectives” course, so I gained a lot of advice from my classmates and professors. One important piece of advice I received was to start with a “hypothesis”. From the beginning, I approached writing and research, with the hypothesis that decreased pathogen abundance was causing increased microbiota diversity and improved lung function, then I started looking to see whether the data in the literature supported or rejected that hypothesis. Reading through the literature with this lens also helped to make sure that I was efficiently including all the relevant studies. The assistance from my labmates and direct help from Dr Goldberg was also essential to the process. I presented the initial proposal for my review during a lab meeting. Their feedback and enthusiasm encouraged me to move forward and helped identify important gaps early in the process. Dr Goldberg made this review possible. With her expertise, she made sure I was correctly reading the literature, provided several studies that I missed in my literature review, sought advice from other experts in the field, and gave direct help with the writing itself.
We uncovered a lot of interesting findings in writing this article. There is a lot that we do not know about ETI therapy and its relationship with the CF lung, but many of the studies were able to provide some insight into particular areas, which creates a clearer overall picture. One consistent finding was that the most dangerous CF pathogens including P. aeruginosa remain present in the CF lung even if their prevalence has decreased. Along with the evolution and genetic changes identified in the bacterial populations, there is a lot to be done regarding the future trajectory of the pathogens in the CF lung.
When discussing my initial motivations for undertaking this topic, I talked about how one of the reasons modulator therapies are so interesting to me is their attempt to solve the underlying problems contributing to disease states. Microbiologists have made remarkable progress on fighting against an evolving enemy, but therapies like ETI and potential wider use of gut microbiota transplants, provide potential future avenues to make sure the most vulnerable are less susceptible to microbial infections rather than fighting the pathogens more directly. I am eager to see what increased multidisciplinary cooperation, more powerful technology, and a new generation of researchers can produce to solve the microbiological problems of tomorrow.
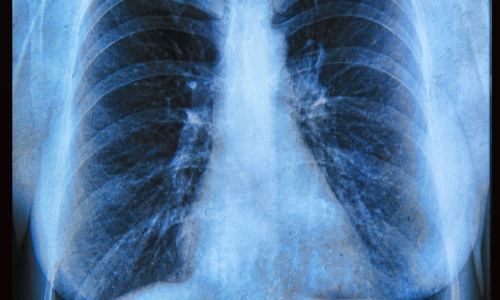
Image: Human lungs infected by virus and bacteria. 3D illustration. iStock/Mohammed Haneefa Nizamudeen
