Jam Talks: phage and the gut microbiome
Posted on February 19, 2020 by Eleanor Townsend
The Junior Awards for Microbiology (JAM Talks) is a monthly seminar series based in Birmingham that allows early career researchers to gain experience presenting to an audience of their peers. Eleanor Townsend, researcher at the University of Warwick, presented her work at the October JAM Talks in 2019. Here Eleanor takes us through her research.
Currently it is difficult to escape news of the coming antibiotic apocalypse. Headlines screaming about “Superbugs”, antibiotic resistance and outbreaks of unstoppable diseases are sadly becoming more and more commonplace.
Many researchers are now frantically looking for alternatives, whether these are sourced from repurposed existing medications, hidden in soil, Komodo dragons or rainforests, or have existed in alternative medicine for centuries. Our research focuses on a different naturally occurring source; viruses that infect bacteria, known as bacteriophage or, more simply, phage.
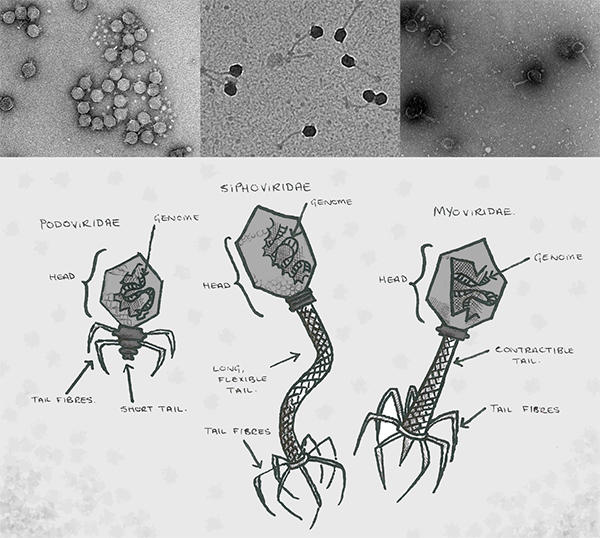
Phage were discovered back in early 1900’s independently by both Felix d'Herelle and Frederick Twort. They exist everywhere in nature and can be found in abundance in soil, sea water, sewage and any other slightly dirty environment you can think of, including the human gut. They have two main lifecycles; lytic (those that kill bacteria straight away) and lysogenic (those that live inside and grow with bacteria). Both lifecycles begin with the phage injecting its genome into a bacterial cell. The lytic cycle has applications for use in phage therapy. Here, after the genome has been injected into the cell, the phage begins to replicate inside by hijacking the bacterial machinery. Once the bacterial cell is stuffed full of new phage, the cell bursts, releasing them to infect further bacteria. In this way, they can clear whole populations of bacteria that may be causing infections.
Phage have been a popular resource for treating infection in countries such as Georgia, Poland and Russia, where currently banks for phage are being created ready to ship to clinicians. Phage have advantages over antibiotics as they are highly specific in which bacteria they infect, meaning there will be no disturbance of the patient’s microbiome. As phage occur naturally and evolve alongside their bacterial hosts, the roles of phage as treatments are potentially unlimited. There is also the option to genetically engineer them as these technologies develop, which could unlock even more uses of phage.
Our current work is looking at using a mixture of these phage (delightfully known as a cocktail) to treat catheter-associated urinary treat infections (CAUTI). To do this, we developed a simple way of modelling the infection in the lab, which involved short sections of catheter in an artificial urine media. We then looked at adding the phage cocktail at different points with antibiotics and whether or not this was able to reduce the number of bacteria.
We found our results varied depending on which antibiotic was chosen alongside the phage cocktail and also when the treatment was applied.
The phage cocktail was particularly effective at preventing the infection from becoming established, but was unable to clear it once the bacterial population had built up into a biofilm. While this may sound like a drawback, there are already many applications (such as plastic bags for lettuce leaves at the supermarket) that have phage fixed to the surface, preventing bacteria from growing and causing food spoilage. This technology could be transferred to a medical appliance, fixing them to the surface of medical devices to prevent bacteria from growing there.
Whilst the phage cocktail worked alone, the combination of antibiotics with phage cocktail was more effective than either treatment alone, an effect known as synergy. This is promising, as combining a phage coated catheter and antibiotics could prevent complications of CAUTI which can be especially deadly in vulnerable patients.
Recently we have started looking at using phage to eliminate unwanted bacteria in the gut microbiome. Some bacteria are able to degrade components of meat and dairy from our diets into compounds which are linked to atherosclerosis, the driving force behind cardiovascular disease. We hope to use phage to target these bacteria only, leaving all good bacteria untouched, therefore reducing the risk of heart disease, one of the leading causes of death worldwide.
The Junior Awards for Microbiology (JAM) talks is a monthly junior seminar series aimed at integrating and connecting young researchers around Europe.

