New antibiotics needed: Haemophilus influenzae
Posted on March 14, 2019 by Laura Cox
In 2017, the World Health Organization (WHO) published the ’12 Priority Pathogens’: a list of twelve microbes that are becoming increasingly resistant to current antimicrobials. These twelve pathogens are thought by WHO to pose the greatest threat to human health.
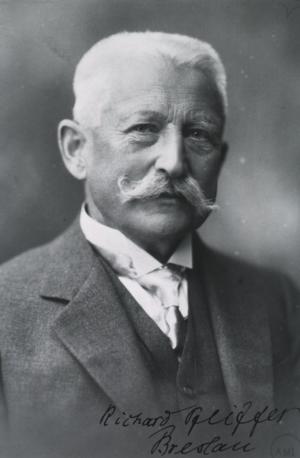
Richard Pfeiffer
Haemophilus influenzae
Haemophilus influenzae was first identified by Richard Pfeiffer in 1892. Formerly known as Pfeiffer’s bacillus, this bacterium was previously thought to be the cause of flu; until influenza virus was determined as the true cause in 1933. Infection with H. influenzae is still sometimes known as bacterial influenza.
In 1992, a vaccine against H. influenzae type B, called the Hib vaccine was introduced in the UK. Since then, the incidence of childhood pneumonia and respiratory tract infections fell, and H. influenzae was almost eradicated in countries that adopted a vaccination programme.
The vaccine works by targeting the major capsule type of H. influenzae, that is, the carbohydrate coating that protects the bacteria from clearance by immune system. Usually, bacterial vaccines such as Hib target proteins in the capsule, enabling the immune system to recognise the bacteria and coordinate an effective immune response.
A re-emerging challenge
It is widely agreed that the Hib vaccine has been a great success. But as vaccine uptake has increased, and rates of H. influenzae type B infection has fallen, infections of a different type of H. influenzae are increasing. Non-typeable H. influenzae (NTHi) cannot be protected by the Hib vaccine due to the lack of a bacterial capsule, and cases of NTHi infection have been rapidly increasing since 2011.
NTHi infection causes a number of painful conditions including a painful infection of the middle ear, chest and throat infections and chronic obstructive pulmonary disease (COPD), which is the third leading cause of death worldwide. COPD is inflammation of the airways and lung damage, presenting as breathlessness, a chesty cough and wheezing from the lungs. Severe cases of NTHi can even lead to sepsis and meningitis, H. influenzae meningitis has a mortality rate of 5% in children, even with treatment.
Rising resistance

Treatment of H. influenzae infection is usually with beta-lactamase antimicrobials, such as ampicillin. Resistance to these antimicrobials in the H. influenzae population is increasing, though, and infections continue to become more difficult to treat.
Some bacteria have intrinsic resistance, meaning they have genes that allow them to tolerate certain antibiotics, against beta-lactams. This intrinsic resistance is now also increasing for other antibiotics, like macrolides. H. influenzae also spreads antimicrobial resistance throughout bacterial populations via plasmids; as intrinsically resistant bacteria survive antibiotic treatment, they can pass the mechanisms for resistance on to susceptible bacteria.
There are reports of H. influenzae isolates even being resistant to Carbapenems, one of the last lines of defence against bacterial infections. This antibiotic is reserved for use only against multi-drug resistant bacterial infections. With the lack of an effective vaccine and rising resistance to the available treatment options, there is a chance that Haemophilus influenzae could return as a major cause of childhood mortality.
The return of Pfeiffer’s bacillus: Rising incidence of ampicillin resistance in Haemophilus influenzae is the fifth review in the New Antibiotics Needed collection in Microbial Genomics. Written by Eva Heinz from the Wellcome Trust Sanger Institute, the review discusses the Hib vaccine coverage around the world and the spread of NTHi throughout Europe. The review also explains the mechanism of resistance to front-line antibiotics in H. influenzae, and urgently calls for a more robust and thorough surveillance of resistant H. influenzae.
More from our New Antibiotics Needed blog series:
Shigella
Salmonella
Enterobacteriaceae
Campylobacter

