Prions, vCJD and the immune system relay
Posted on December 2, 2013 by Benjamin Thompson
Despite more than a decade’s worth of research, many aspects of variant Creutzfeldt–Jakob disease (vCJD) still remain a mystery. This fatal neurodegenerative disease of the brain is often referred to as the human form of bovine spongiform encephalopathy (BSE), known to most as ‘mad cow disease’.
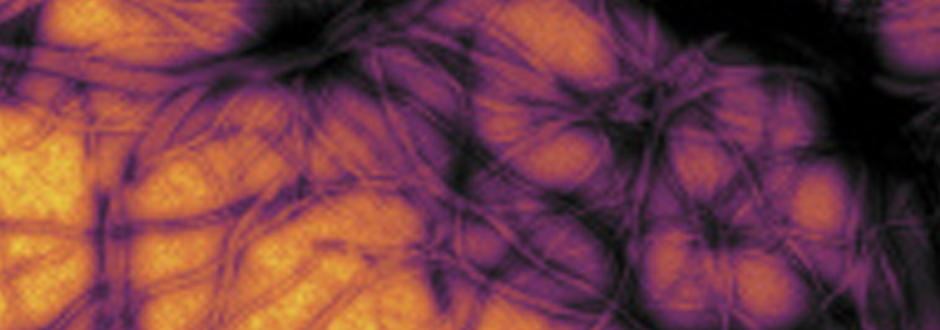
vCJD was first described in 1986 and was attributed to humans eating meat from infected cattle. The exact root of the disease is still unknown, but proteins known as prions are believed to be the causative agent. A build up of misfolded prions in the brain causes the progressive death of neurons, for which there is no cure. The brains of people that have died of the disease look sponge-like when viewed under a microscope, hence the word ‘spongiform’ in BSE.
Misfolding proteins
The way that a prion infection spreads is debated. The prion mode of action is very different to bacteria and viruses as they are simply proteins, devoid of any genetic material. Once a misfolded prion enters a healthy person – potentially by eating infected food – it converts correctly-folded proteins into the disease-associated form. To date, nobody knows quite how this happens.
vCJD is by no means the only form of prion disease in humans. Sporadic CJD (sCJD) is the most common, causing around 1-2 deaths per 1,000,000 people in the UK each year, generally in those over the age of 60. vCJD is also rare – despite an estimated 400-500,000 BSE infected cattle entering the food chain in the 1980’s – with only 177 definite or probable cases having been reported to date. Unlike sCJD, the majority of those affected were young (~26 years old).
Initially, this age discrepancy was thought to be related to dietary habits, with young people more likely to be eating food with a high risk of contamination. No strong evidence for this was found (old people eat pies and burgers, too).
The immune system relay
New research from scientists at The Roslin Institute, University of Edinburgh, published in the Journal of General Virology, is helping us to understand why vCJD appears to mainly affect the young.
Having a healthy immune system seems to be central to vCJD development. Indeed, mice that lack a functional immune system have a lower susceptibility to prion disease. The misfolded prions appear to hijack the defence system that protects against bacterial and viral infection, using it to gain access to the nervous system and, ultimately, the brain.
Dr Neil Mabbott, one of the co-authors of the study, describes the movement of the prions as ‘a relay’, which begins in the small intestine.
In order to ascertain whether there are any pathogens in the small intestine and, if so, what response needs to be mounted, the body uses an ‘antigen sampling’ system (kind of a built in dipstick) to see what is present.
This system is the point of entry for the misfolded prions, allowing them to slip in the body’s lymphatic system. Once there, they attach to the surface of immune cells known as follicular dendritic cells (FDCs), and replicate by causing normal prion proteins to misfold into the disease-causing version.
Through methods unknown, the misfolded prions escape the surface of the FDCs, moving into the nerves, and spread through the spinal cord and vagus nerve to the brain where the real damage begins.
The new research studied two groups of mice: 32 between six and eight weeks of age and 29 around ninety weeks old (very old for a mouse). These two groups of mice were injected with prions from a cow known to have been infected with BSE.
Dropping the baton?
Within a few months, prions had accumulated in the lymph nodes and spleen of the young mice, although they did not show any signs of disease. Over a year later, the majority of those tested showed classic signs of prion neurodegeneration.
In contrast, none of the old mice developed any clinical disease, all died of natural age-related diseases. Only one of the 29 older aged mice showed any sign of having prions in its brain and this was only in a small, localised area. Given that most of these adult mice died before the time it takes to develop prion disease, it can’t be ruled out that they would have developed an infection if they’d lived long enough, although there was no evidence of any prion-related neurodegeneration.
Despite there being no evidence of prions in the elderly mice’s brains, there were detectable levels in their spleens, albeit at lower levels than in the younger mice. Dr Mabbott suggests that this may be because one of the relay steps is missing, or working less efficiently, in the older mice.
The research, funded by the BBSRC and the EU-FP7, builds on previous work that showed how the microarchitecture of the mice’s spleen – part of the antigen sampling system – deteriorates with age, as do the numbers of FDCs, leaving less for the prions to replicate on.
Error bars
While this study does provide us with further background into vCJD, a disease that remains much of a mystery, we need to remember that the mice being used in the study are clearly not humans, so any parallels drawn between the two species must be done carefully. That said, recent research published in the BMJ suggests that levels of abnormal vCJD prions in humans appear to be higher than we previously thought.
Researchers investigated over 30,000 stored appendix samples, removed during operations in the UK between 2000 and 2012, of which 16 showed evidence of abnormal prions. Although a small number, the authors of the paper suggest that this indicates a prevalence of 493 people per million in the UK with abnormal prions, higher than the total number of confirmed vCJD cases (177) to date.
In addition to showing the importance of ageing to susceptibility of prion disease, Dr Mabbott’s work has also uncovered the effects that getting old has on the immune system. He has recently been awarded a grant from the BBSRC to further investigate the mechanisms that cause the immune system to break down, which may ultimately help to improve people’s health as they get older.
References
Brown KL, & Mabbott NA (2013). Evidence of sub-clinical prion disease in aged mice following exposure to bovine spongiform encephalopathy. Journal of General Virology DOI: 10.1099/vir.0.058958-0
Valleron AJ, Boelle PY, Will R, & Cesbron JY (2001). Estimation of epidemic size and incubation time based on age characteristics of vCJD in the United Kingdom. Science, 294(5547), 1726-8 : 10.1126/science.1066838
Boëlle PY, Cesbron JY, & Valleron AJ (2004). Epidemiological evidence of higher susceptibility to vCJD in the young. BMC infectious diseases, 4, 26-32 : 10.1186/1471-2334-4-26
Brown KL, Stewart K, Bruce ME, & Fraser H (1997). Severely combined immunodeficient (SCID) mice resist infection with bovine spongiform encephalopathy. Journal of General Virology, 78, 2707-10 PMID: 9349494
Gill ON, Spencer Y, Richard-Loendt A, Kelly C, Dabaghian R, Boyes L, Linehan J, Simmons M, Webb P, Bellerby P, Andrews N, Hilton DA, Ironside JW, Beck J, Poulter M, Mead S, & Brandner S (2013). Prevalent abnormal prion protein in human appendixes after bovine spongiform encephalopathy epizootic: large scale survey. BMJ, 347 : 10.1136/bmj.f5675

