New antibiotics needed: Pseudomonas aeruginosa
Posted on September 17, 2020 by Laura Cox
In 2017, the World Health Organization (WHO) published the ’12 Priority Pathogens’: a list of 12 microbes that are becoming increasingly resistant to current antimicrobials. These 12 pathogens are thought by WHO to pose the greatest threat to human health.

An adaptable pathogen
Pseudomonas aeruginosa is one of the few types of bacteria which can cause disease in both animals – including people – and plants, particularly lettuce. This species of bacteria is highly prevalent and can be found in numerous natural environments, such as soil and water; as part of the natural flora of skin and in most man-made environments. P. aeruginosa can use a wide range of organic materials for nutrition and is able to thrive in normal and low levels of oxygen, meaning it is able to live in diverse environments.
This rod-shaped bacterium is of particular medical importance as it is associated with numerous healthcare-associated infections and is considered an opportunistic pathogen, as it is capable of causing serious disease in those with existing conditions. A particular area of concern is P. aeruginosa infection in people with cystic fibrosis or people with burns. Infections can result in inflammation and sepsis. If the bacteria colonise the lungs, kidney or urinary tract, the results can be fatal.
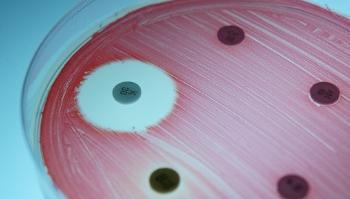
Naturally resistant
P. aeruginosa is considered a model organism for antibiotic resistance due to its large genome. This extensive genome includes a range of mechanisms of antimicrobial resistance. These bacteria possess efflux pumps, which are capable of pumping a range of antibiotics out of the cell. In addition, they produce a number of enzymes which are capable of degrading or inactivating any antibiotic molecules within the cell.
As with many of the WHO Priority Pathogens, P. aeruginosa is capable of sharing antibiotic resistance traits by horizontal transfer. This means that if one strain of bacteria mutates and becomes resistant to a certain antibiotic, it can package up the genetic material that enables this resistance and share it with nearby bacteria, which may not share the same trait.
Endurance over virulence
P. aeruginosa employs a wide range of tactics to establish persistent, long-term infection in the host. This comes at a cost though, with the bacteria trading off virulence factors to prioritise the traits that allow longer term infections. In immunocompromised people, such as those with cystic fibrosis, clearing these chronic infections with antibiotics can seem impossible, with higher and higher doses needed. With this comes another set of challenges, as the adverse effects of treatments can severely affect quality of life.
In their review ‘Antibiotic resistance in Pseudomonas aeruginosa and adaptation to complex dynamic environments,’ Lea Sommer, Helle Johansen and Søren Molin explore the challenges in using genomic data to predict the characteristics of P. aeruginosa. This open-access review, published in the journal Microbial Genomics, is the twelfth and final paper in the New Antibiotics Needed collection.