Investigating the possible role of L-form switching in recurrent urinary tract infections

The Microbiology Society is undertaking a project entitled A Sustainable Future as part of our 75th Anniversary, which aims to highlight the Sustainable Development Goals (SDGs) to our members and empower them to use their research to evidence and impact the goals. Earlier this year, we put a call out to our members to submit case studies in the following three areas: antimicrobial resistance, soil health and the circular economy.
This case study is written by Dr Katarzyna Mickiewicz, who is a Faculty of Medical Sciences Research Fellow at the University of Newcastle, UK, and a member of the Microbiology Society. It focuses on antimicrobial resistance; a naturally occurring process, whereby micro-organisms (bacteria, viruses, fungi and parasites) can change and adapt over time, either by modifying the target of the antimicrobial, or by developing and exchanging resistance genes.
What are the challenges/needs that this research addresses?
Antimicrobial resistance (AMR) is a major concern within clinical settings and in farming. My research focuses on a mechanism of antibiotic evasion, called L-form switching. This process involves a transient loss of a bacterial protective layer, called the cell wall, in response to antibiotics that target this structure. Without the wall, bacteria lose their shape, become susceptible to bursting and slow growing, but they can survive if the surrounding environment provides sufficient osmoprotection. Once antibiotics are gone, bacteria can rebuild the wall and resume rapid growth (Figure 1). Importantly, many pathogens, including Escherichia coli and Staphylococcus aureus, are able to undergo L-form switching and this mechanism has been implicated in recurrence of several diseases, including sepsis, mastitis, urinary tract and gastrointestinal infections, both in human and animals1-7. However, the fragile nature of L-forms and their slow growth make them very difficult to study in the host’s body. It is hard to isolate L-forms and differentiate them in situ from structures of eukaryotic origin due to their polymorphic appearance. As a consequence, L-form switching in the context of the host is poorly understood, even though the mechanism potentially provides a powerful strategy for the evasion of some of our best and most commonly used antibiotics, such as β-lactams.
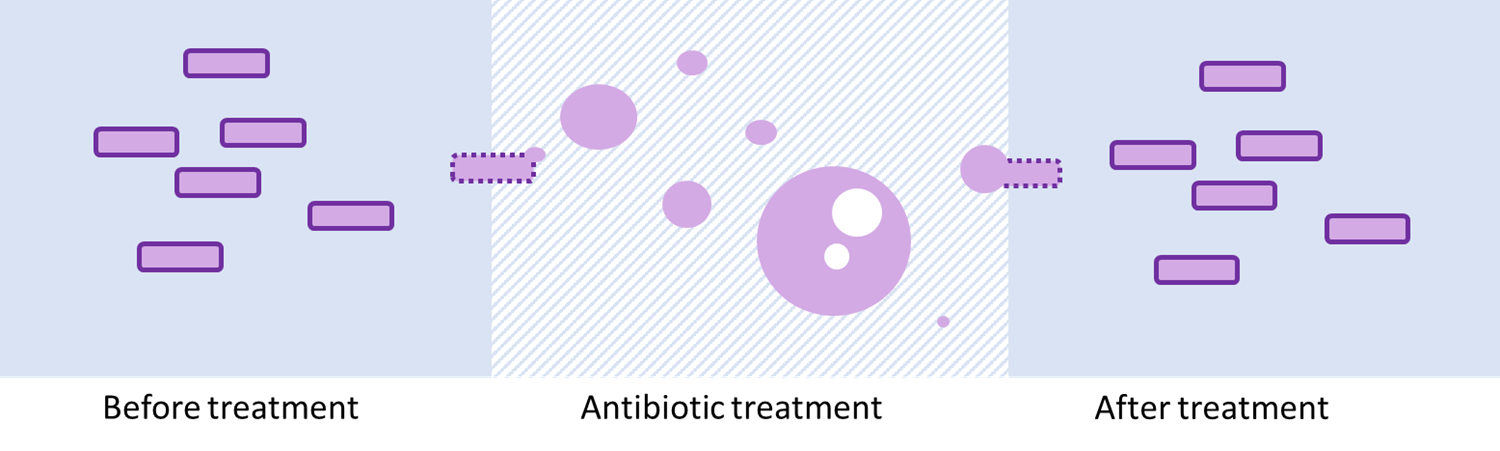
Figure 1) L-form switching as a mechanism for bacterial recurrence. Bacteria treated with cell-wall-targeting antibiotics lose the cell wall, which leads to emergence of L-forms. Following antibiotic treatment, the bacteria can regenerate the wall and potentially cause recurrence of a full-blown infection. The bacterial cell wall is indicated with dark purple lines. Figure adapted from7.
What findings and solutions were provided by this research?
To demonstrate that L-forms are able to exist in the context of human hosts, urine samples donated by patients with recurrent urinary tract infections were examined by phase contrast microscopy for the presence of L-form-like structures7. For the positive samples, this was followed by fluorescence in situ hybridisation (FISH) with a fluorescently labelled oligonucleotide probe, which binds specifically to a bacterial 16S rRNA sequence. This confirmed the observed structures were indeed of bacterial origin. Urine samples were also filtered through a 0.45 µm filter, which allowed passage of cell-wall deficient bacteria, but not walled bacterial forms. Using this method, a range of bacterial species capable of L-form switching in the host were isolated, including E. coli, Enterococcus spp., Streptomyces spp., Staphylococcus spp., and Klebsiella spp. E. coli isolates expressing cytoplasmic fluorescent markers were used to show directly (in vitro and in the zebrafish model Danio rerio) the switching to L-forms in the presence of cell wall-targeting antibiotics and subsequent reversion to walled forms following antibiotic withdrawal. Collectively, these experiments demonstrate that L-form switching is a physiologically relevant phenomenon, which can contribute to evasion of cell wall-targeting antibiotics.
How can this research support the transition to a more sustainable future?
In the era of rising antimicrobial resistance (AMR), it is crucial to understand precisely how antibiotics work in the context of the host, rather than solely under artificial in vitro conditions. Moreover, to solve complex cases of recurrent infection, which particularly affect elderly or immunocompromised patients, we need to understand not only the most common bacterial responses to antibiotics on a whole population level, but also rare events, on a single cell level. Although studying L-form switching in the host is challenging, it brings novel insights into how cell wall-targeting antibiotics work in vivo. It has the potential to influence how to use currently available treatments better, as well as develop novel strategies for tackling infections.
What is the future for research and innovation in this area?
Many questions regarding L-form switching remain unanswered. It is still unknown to what extent L-form switching contributes to recurrence of infections and how it compares with other mechanisms of antibiotic evasion. What are the precise locations within a host; which are favourable for L-form survival? Do they prefer intracellular or extracellular environments? And most importantly, how can they be eradicated? Methods such as advanced fluorescence microscopy, combined with optically accessible infection models, will bring us closer to the answers. Modifying drug testing conditions, so they are supportive of L-form survival, will be important to establish which drugs are effective against L-forms. Consolidated effort from research groups across the globe is needed to establish the impact of L-form switching on various infectious diseases.
References
- Domingue, G. J. Sr. & Woody, H. B. Bacterial persistence and expression of disease. Clin. Microbiol. Rev. 10, 320–344 (1997).
- Domingue, G. J. Demystifying pleomorphic forms in persistence and expression of disease: Are they bacteria, and is peptidoglycan the solution? Discov. Med. 10, 234–246 (2010).
- Allan, E. J., Hoischen, C. & Gumpert, J. Bacterial L-forms. Adv. Appl. Microbiol. 68, 1–39 (2009).
- Onwuamaegbu, M. E., Belcher, R. A. & Soare, C. Cell wall-deficient bacteria as a cause of infections: a review of the clinical significance. J. Int. Med. Res. 33, 1–20 (2005).
- Clasener, H. Pathogenicity of the L-phase of bacteria. Annu. Rev. Microbiol. 26, 55–84 (1972).
- Errington, J., Mickiewicz, K., Kawai, Y. & Wu, L. J. L-form bacteria, chronic diseases and the origins of life. Philos. Trans. R. Soc. Lond. B Biol. Sci. 371, 20150494 (2016).
- Mickiewicz, K.M., Kawai, Y., Drage, L. et al. Possible role of L-form switching in recurrent urinary tract infection. Nat Commun 10, 4379 (2019).

About the author
Dr Katarzyna Mickiewicz, who is a Faculty of Medical Sciences Research Fellow at the University of Newcastle and a member of the Microbiology Society. More information about her work is available here.


